Alternative uses of EtCO2 in the pre-hospital and critical care settings
End-tidal capnography in clinical practice originated in the field of anesthesia around the 1950s but has also become established in the pre-hospital setting. EMS providers commonly use end-tidal CO2 values as an adjunct to cardiac arrest and airway management. Continuing to learn about end-tidal CO2 is critical because this device is easily applied, readily available, and relatively cheap. Recent literature illustrates an expanded role of end-tidal CO2 in differentiating respiratory ailments, sepsis care, trauma management, and predicting medical complications.
Overview
In this article, we will review the uses of EtCO2 in cardiac arrest and discuss new methods from recent literature. We will focus on quantitative EtCO2, which produces both a value and a waveform.
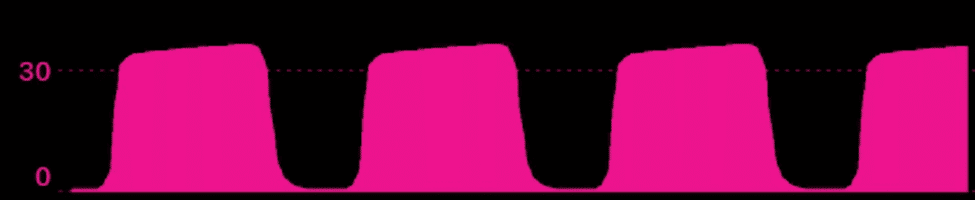
Figure 1.1: Cardiac Arrest Management
EtCO2 relies on three primary factors: tissue CO2 production, pulmonary blood flow, and alveolar ventilation. In low-flow states such as cardiac arrest, pulmonary perfusion becomes the primary determinant of EtCO2 values. Therefore, EtCO2 helps determine chest compression effectiveness, ROSC prediction and detection, resuscitation termination, and repeat episodes of cardiac arrest.
Chest compressions are one of the few interventions that increase the likelihood of functional survival from out-of-hospital cardiac arrest (OHCA). Based on this information, we must have monitoring devices that evaluate the effectiveness of this intervention.
Observational clinical research suggests that increased chest compression depth, rate, and release velocity are related to a statistically significant increase in EtCO2. Conversely, an increased ventilation rate was associated with decreased EtCO2 (1). The data size within this study was clinically modest, but it provides preliminary support that EtCO2 may be used to monitor chest compression effectiveness and limit hyperventilation. This study is supported by new research, which shows optimization of chest compression release velocity is associated with higher EtCO2 values. This is important because higher EtCO2 values are associated with improved outcomes in OHCA (2). Additionally, recent literature using transthoracic echocardiograms in the pre-hospital setting has shown an association between ventricular compression and EtCO2 values (3).
Factors including minute volume, underlying etiology, medications, and existing conditions impact the overall EtCO2 value in cardiac arrest, but the trend remains useful. For example, if compressors switched during the last rhythm analysis and now EtCO2 values are lower, the new compressor may require coaching or should be switched out with another team member. Close monitoring for any changes in CPR effectiveness is critical as the literature suggests the quality of compressions deteriorates before subjective fatigue sets in (4).
EtCO2 values during a cardiac arrest have been cited for their prognostic significance. Research has shown higher values of EtCO2 are related to increased ROSC incidence (5,6,7). Additional research that evaluated patients in non-shockable rhythm OHCA illustrates a relationship between high initial EtCO2 levels (> 45 mmHg) and 30-day survival (8). Therefore, capnography may be a helpful prognostic tool even in patients with factors traditionally indicative of reduced survival, including unwitnessed arrest, no bystander CPR, and non-shockable rhythms. Furthermore, the absolute maximum value of EtCO2 is also associated with predicting ROSC in cardiac, respiratory, and traumatic etiologies (9). Conversely, profound hypocapnia (<10 mmHg) following 20 minutes of resuscitation indicates a poor prognosis and can be helpful in the termination of resuscitation (5,10).
Lastly, abrupt changes in EtCO2 can be clinically significant. Studies have shown a sharp increase in EtCO2 during CPR is specific to ROSC (11). This finding indicates the need to perform a rhythm analysis, pulse check, and potentially prepare for post-resuscitation care. Conversely, an abrupt decrease in EtCO2 may mean reduced perfusion caused by a re-arrest state. A reduction in EtCO2 has also been shown to predict in-hospital cardiac arrest, making it a valuable tool for preparing for patient decompensation (12). Ultimately, any changes in EtCO2 values indicate a possible clinical development requiring thorough reassessment.
Effective Airway/Ventilatory Management
Continuous waveform capnography is the gold standard for pre-hospital intubation confirmation. Successful endotracheal intubation should correlate with consistent waveform morphology during each ventilation (13). Capnography is sufficient in intubation confirmation even in low flow states and cadavers. For example, experimental research on human cadavers illustrated endotracheal tube confirmation with 100% sensitivity and specificity (14). As described above, an abrupt loss in EtCO2 is a critical finding and requires assessment. Besides cardiac arrest or profound hypoperfusion, an abrupt loss of EtCO2 values can also be caused by ET tube dislodgement or a complication with the EtCO2 line (13).
Furthermore, EtCO2 helps identify hypoventilation following analgesia or sedation. EtCO2 will begin showing hypoventilation (figure 1.2), and CO2 retention before a pulse oximeter indicates hypoxemia (15,16). In patients that require positive-pressure ventilation, capnography helps track ongoing ventilatory rates. Hyperventilation leads to complications such as barotrauma, gastric distention with subsequent aspiration, increased intrathoracic pressure, decreased venous return, and reduced cardiac output (13,16). Initial evidence of hyperventilation may include displayed ventilatory rates higher than optimal or a gradual decline in EtCO2 values without hemodynamic change.
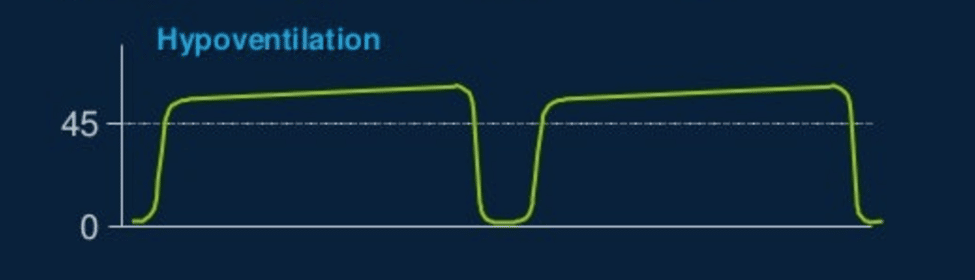
Figure 1.2: Hypoventilation
Another phenomenon that EtCO2 helps assess is breath stacking. As shown below, the EtCO2 waveform will begin to show hypercapnia and morphology that does not return to the respiratory baseline. This complication may arise from a reduction in expiratory time where a complete exhalation does not occur before the next inspiration begins. Patients that require a prolonged expiratory phase, such as those with COPD and asthma, are at high risk for this condition. Similar to hyperventilation, these patients are at risk for barotrauma or reduced cardiac output from increased intrathoracic pressure. In patients undergoing mechanical ventilation, settings may need to be adjusted to reduce the prevalence of this complication. For example, a reduction in ventilatory rate and inspiratory time allows more time for complete exhalation, see figure 1.3 below.
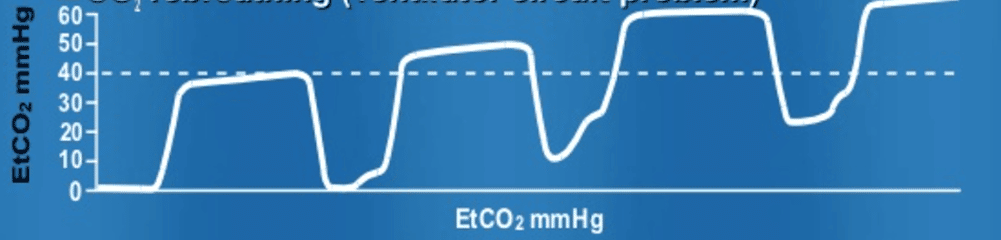
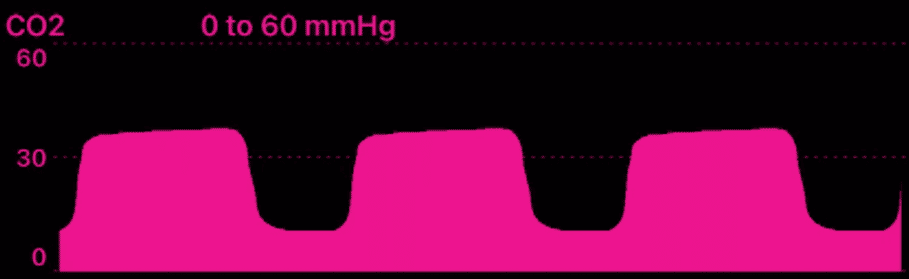
Figure 1.3: Rebreathing – Reduction in expiratory phase
Additionally, if a patient has incomplete paralysis or leak, they will likely show a curare cleft waveform as shown in figure 1.4. The curare cleft waveform will help you detect breakthrough breathing or more commonly a leak within the circuit.
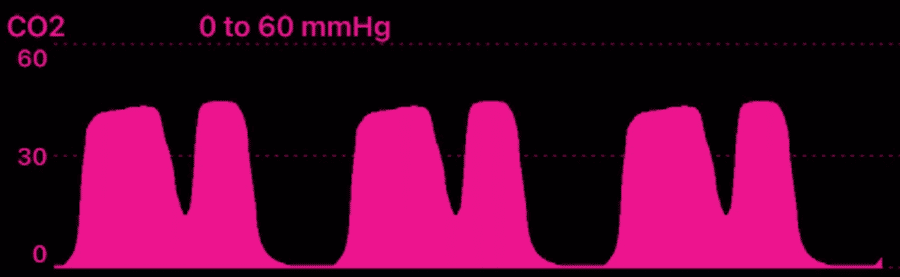
Figure 1.4: Curare cleft waveform – Incomplete paralysis or leak
Sepsis
One of the primary objectives of pre-hospital sepsis care is identification. Recent literature suggests that qSOFA criteria are not as sensitive for sepsis as we once believed. As a result, current recommendations indicate transitioning to SIRS criteria (17). One complication with both qSOFA and SIRS criteria is low specificity causing a significant number of false sepsis activations. Hunter et al. (2016) examined the effect of adding an EtCO2 level < 25 mmHg to SIRS criteria for the identification of sepsis (18). They found that EtCO2 was the strongest predictor of sepsis, severe sepsis, and mortality. Therefore, implementing EtCO2 can increase the accuracy of sepsis screening and reduce the number of false activations.
The progression of sepsis leads to hemodynamic changes requiring timely management. First-line treatment includes intravenous fluids, antibiotic administration, and vasopressors as needed to maintain end-organ perfusion. It is crucial to assess the fluid responsiveness of sepsis patients to ensure appropriate amounts of intravenous fluids are provided. One method of determining fluid responsiveness is assessing cardiac output variation in the presence of passive leg raises (PLR). A cardiac output variation of 15% during PLR is defined as fluid responsive. In the absence of invasive cardiac measurements, EtCO2 can be used as a surrogate for cardiac output and fluid responsiveness during PLR maneuvers. For example, Toupin et al. illustrate an increase in EtCO2 by two mmHg is associated with fluid responsiveness in hemodynamically stable cardiac surgery patients (19). A more recent systematic review indicates that an increased EtCO2 by two mmHg or more has a high specificity and sensitivity for fluid responsiveness in ICU, OR, or mechanically ventilated patients (20).
Trauma
Recent literature illustrates a relationship between low EtCO2 values in trauma patients and the need for surgery or blood transfusion (21). In addition, research in pediatric patients identified an association between triage EtCO2 < 35 mmHg and elevated lactate, positive FAST, a need for blood transfusions, and operative intervention (22). Further, early literature suggests that EtCO2 is a better predictor of mortality and the need for massive transfusion than systolic blood pressure and shock index (23,24). As a result, pre-hospital providers should include this assessment tool and report it when providing trauma alerts. Pending further research, end-tidal capnography may be a practical addition to trauma designation protocol.
The Excellence in Prehospital Injury Care (EPIC) study by the University of Arizona identified three “H bombs” associated with a significant increase in mortality and morbidity. These include hypoxia, hypotension, and hyperventilation (25). Hyperventilation, which can be assessed effectively with EtCO2, is related to cerebral vasoconstriction and ischemia (26). Therefore, EtCO2 can be applied to all head trauma patients requiring airway/ventilatory support to ensure that providers maintain tight control of EtCO2 and avoid hyperventilation. EPIC suggests that EtCO2 values are targeted at around 40 mmHg to optimize the outcome of head trauma patients (25).
Lastly, EtCO2 may be an easily deployable vital sign in a mass casualty incident. For example, it can be challenging to determine who is transported first when multiple patients meet the emergent category. Triage EtCO2 may help predict the most critical patients that will likely require emergent surgery and transfusion in this case.
Identification of Diabetic Ketoacidosis
One of the hallmarks of diabetic ketoacidosis (DKA) includes Kussmaul respirations, which are characterized by deep, rapid breathing. In DKA, ketone bodies are produced in high amounts as a protective mechanism against cellular starvation. However, the over-production of ketones leads to metabolic acidosis (27). One of the compensatory mechanisms of this effect is to increase the minute volume, as seen in Kussmaul respirations. This event causes a drastic reduction in PaCO2, attempting to realign the Henderson-Hasselbalch Equation for the bicarbonate buffer (28). EtCO2 monitoring of a patient in DKA may illustrate profound tachypnea, high tidal volumes, and hypocapnia. Therefore, EtCO2 monitoring is helpful in the identification of DKA and also patient progression during longer transports.
Differentiation of Respiratory Pathology
Everyone that has been in EMS for a bit can validate that patients do not commonly fit textbook criteria. Patients will likely have multiple co-existing respiratory conditions that complicate the differential diagnosis. EtCO2 can help provide information to support specific pathologies during respiratory distress. For example, bronchospasm, commonly associated with COPD or asthma, frequently illustrates a shark-fin morphology due to an extended expiratory phase. As a result of incomplete exhalation, these patients will begin to retain CO2 and commonly show signs of hypercapnia. COPD and asthma patients frequently receive beta-adrenergic medications with the desired effect of bronchodilation. The EtCO2 morphology can be used to assess the effectiveness of these medications over time. As bronchodilation occurs, we expect less profound shark-fin morphology and a reduction in EtCO2 values.
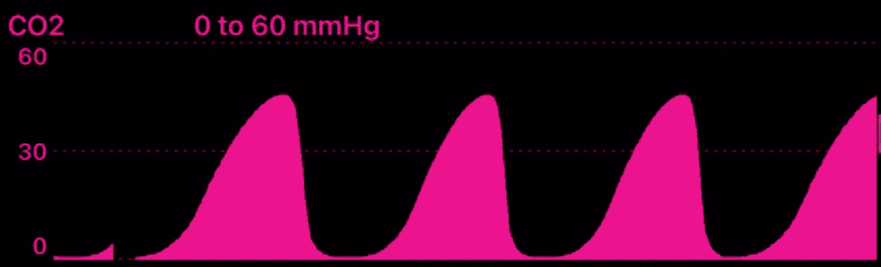
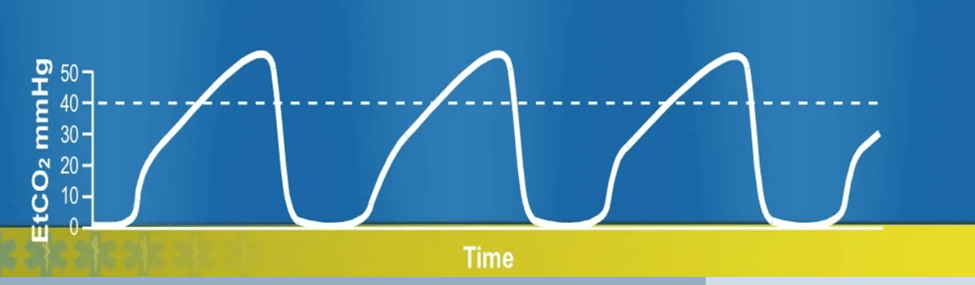
Figure 1.5: Shark fin morphology
On the contrary, patients with respiratory distress associated with congestive heart failure (CHF) commonly have hypocapnia and normal waveform capnography while they are still compensating. Hunter et al. (2015) performed a retrospective study using pre-hospital EtCO2 for patients transported for either COPD or CHF. The results illustrated a cut-off value of < 40 mmHg was 93% sensitive for CHF (29). However, as patients develop respiratory failure, we may see an alarming increase in EtCO2, indicating the need for emergent therapy. Pulmonary embolisms (PEs) frequently present with hypocapnia and normal waveform morphology. EtCO2 has been used as a surrogate for dead space ventilation in patients with PE. Evidence suggests that EtCO2 can be used as a screening tool for PE as patients will likely present with significantly lower EtCO2 values (30, 31). Therefore, EtCO2 may be a tool added to increase diagnostic accuracy and reduce the risk of unnecessary CTPAs.
Conclusion
Overall, end-tidal capnography is an easily deployable vital sign that may provide critical insight into various pathologies. The application of end-tidal CO2 assists in monitoring cardiac arrest care, confirming airway placement, maintaining tight control of ventilatory rates, triaging trauma patients, differentiating respiratory conditions, and identifying metabolic disorders including sepsis and DKA.
References
[1] Murphy, R. A., Bobrow, B. J., Spaite, D. W., Hu, C., McDannold, R., & Vadeboncoeur, T. F. (2016). Association between prehospital CPR quality and end-tidal carbon dioxide levels in out-of-hospital cardiac arrest. Prehospital Emergency Care, 20(3), 369-377. https://doi.org/10.3109/10903127.2015.1115929
[2] Roos, E. D., Vanwulpen, M., & Hachimi-Idrissi, S. (2022). Chest compression release velocity: An independent determinant of end-tidal carbon dioxide in out-of-hospital cardiac arrest. American Journal of Emergency Medicine, 54, 71-75. https://doi.org/10.1016/j.ajem.2022.01.053
[3] Skulec, R., Vojtisek, P., & Cerny, V. (2019). Correlation between end-tidal carbon dioxide and the degree of compression of heart cavities measured by transthoracic echocardiography during cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Critical Care, 23(1). https://doi.org/10.1186/s13054-019-2607-2
[4] Yang, Z., Li, H., Yu, T., Chen, C., & Huang, Z. (2013). The quality of hands-only CPR deteriorates in one minute but without subjective fatigue of rescuer [Abstract]. Critical Care Medicine, 41(12), 117. https://journals.lww.com/ccmjournal/Abstract/2013/12001/480__THE_QUALITY_OF_HANDS_ONLY_CPR_DETERIORATES_IN.442.aspx
[5] Ozturk, F., Parlak, I., Yolcu, S., Tomruk, O., Erdur, B., Kilicaslan, R., Miran, A. S., & Akay, S. (2014). Effect of end-tidal carbon dioxide measurement on resuscitation efficiency and termination of resuscitation. Turkish Journal of Emergency Medicine, 14(1), 25-31. https://doi.org/10.5505/1304.7361.2014.65807
[6] Crickmer, M., Drennan, I. R., Turner, L., & Cheskes, S. (2021). The association between end-tidal CO2 and return of spontaneous circulation after out-of-hospital cardiac arrest with pulseless electrical activity. Resuscitation, 167, 76-81. https://doi.org/10.1016/j.resuscitation.2021.08.014
[7] Hartmann, S. M., Farris, R. W., Gennaro, J. L., & Roberts, J. S. (2015). Systematic review and meta-analysis of end-tidal carbon dioxide values associated with return of spontaneous circulation during cardiopulmonary resuscitation. [Abstract]. Journal of Intensive Care Medicine, 30(7), 426-435. https://doi.org/10.1177/0885066614530839
[8] Poppe, M., Stratil, P., Clodi, C., Schriefl, C., Nurnberger, A., Magnet, I., Warenits, A., Hubner, P., Lobmeyr, E., Schober, A., Zajicek, A., & Testori, C. (2019). Initial end-tidal carbon dioxide as a predictive factor for return of spontaneous circulation in nonshockable out-of-hospital cardiac arrest patients. European Journal of Anaesthesiology, 36, 524-530. https://doi.org/10.1097/eja.0000000000000999
[9] Javaudin, F., Her, S., Le Bastard, Q., De Carvalho, H., Le Conte, P., Baert, V., Hubert, H., Montassier, E., Lascarrou, J., Leclere, B., Reac, G. (2020). Maximum value of end-tidal carbon dioxide concentrations during resuscitation as an indicator of return of spontaneous circulation in out-of-hospital cardiac arrest. Prehospital Emergency Care, 24(4), 478-484. https://doi.org/10.1080/10903127.2019.1680782
[10] Paiva, E. F., Paxton, J. H., & O’Neil, B. J. (2018). The use of end-tidal carbon dioxide measurement to guide management of cardiac arrest: A systematic review. [Abstract]. Resuscitation, 123, 1-7. https://doi.org/10.1016/j.resuscitation.2017.12.003
[11] Lui, C. T., Poon, K. M., Tsui, K. L. (2016). Abrupt rise of end tidal carbon dioxide level was a specific but non-sensitive marker of return of spontaneous circulation in patient with out-of-hospital cardiac arrest. Resuscitation, 104, 53-58. https://doi.org/10.1016/j.resuscitation.2016.04.018
[12] Mucksavage, J. J., He, K. J., Chang, J., Panlilio-Villanueva, M., Wang, T., Fraidenburg, D., & Benken, S. T. (2020). A pilot study of end-tidal carbon dioxide in prediction of inhospital cardiac arrests. Critical Care Explorations, 2(10). https://doi.org/10.1097/cce.0000000000000204
[13] Carlson, J. N., Colella, M. R., Daya, M. R., De Maio, V. J., Nawrocki, P., Nikolla, D. A., & Bosson, N. (2022). Prehospital cardiac arrest airway management: An NAEMSP position statement and resource document. Prehospital Emergency Care, 26(1), 54-63. https://doi.org/10.1080/10903127.2021.1971349
[14] Silvestri, S., Ladde, J. G., Brown, J. F., Roa, J. V., Hunter, C., & Ralls, G. A. (2017). Endotracheal tube placement confirmation: 100% sensitivity and specificity with sustained four-phase capnographic waveforms in a cadaveric experimental model. Resuscitation, 115, 192-198. https://doi.org/10.1016/j.resuscitation.2017.01.002
[15] Li, M., Liu, Z., Lin, F., Wang, H., Niu, X., Ge, X., Fu, S., Fang, L., & Li, C. (2018). End-tidal carbon dioxide monitoring improves patient safety during propofol-based sedation for breast lumpectomy. European Journal of Anesthesiology, 35(11), 848-855. https://doi.org/10.1097/eja.0000000000000859
[16] Lyng, J. W., Guyette, F. X., Levy, M., & Bosson, N. (2022). Prehospital mechanical ventilation: An NAEMSP position statement and resource document. Prehospital Emergency Care, 26(1), 23-31. https://doi.org/10.1080/10903127.2021.1981506
[17] Evans, L., Rhodes, A., Alhazzani, W., Antonelli, M., Coopersmith, C. M., French, C., Machado, F. R., Mcintyre, L., Ostermann, M., Prescott, H. C., Schorr, C., Simpson, S., Wiersinga, W. J., Alshamsi, F., Angus, D. C., Arabi, Y., Azevedo, L., Beale, R., Beilman, G., Belley-Cote, E., Burry, L.,…Levy, M. (2021). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Medicine, 47(11), 1181-1247. Doi: https://doi.org/10.1007%2Fs00134-021-06506-y
[18] Hunter, C. L., Silvestri, S., Ralls, G., Stone, A., Walker, A., & Papa, L. (2016). A prehospital screening tool utilizing end-tidal carbon dioxide predicts sepsis and severe sepsis. American Journal of Emergency Medicine, 34(5), 813-819. https://doi.org/10.1016/j.ajem.2016.01.017
[19] Toupin, F., Clairoux, A., Deschamps, A., Lebon, J., Lamarche, Y., Lambert, J., Fortier, A., & Denault. A. Y. (2016). Assessment of fluid responsiveness with end-tidal carbon dioxide using a simplified passive leg raising maneuver: A prospective observational study. Canadian Journal of Anesthesia, 63, 1033-1041. https://doi.org/10.1007/s12630-016-0677-z
[20] Oberg, E. B., Jorgensen, B. G., Berthelsen, P. G. (2019). End-tidal CO2 in the diagnosis of fluid responsiveness – a systematic review. Danish Medical Journal, 66(9). PMID: 31495370
[21] Wilson, B. R., Bruno, J., Duckwitz, M., Akers, N., Jeanmonod, D., & Jeanmonod, R. (2021). Prehospital end-tidal CO2 as an early marker for transfusion requirement in trauma patients. American Journal of Emergency Medicine, 45, 254-257. https://doi.org/10.1016/j.ajem.2020.08.056
[22] Melvin, J., Meltzer, J., Lewis, E., Villanueva, J., Reddy, S., Chao, E., & Stone, M. (2020). Triage end-tidal CO2 in pediatric trauma: A marker for hemorrhagic shock and operative intervention. [Abstract]. Critical Care Medicine, 48(1), 825. https://journals.lww.com/ccmjournal/Citation/2020/01001/1700__TRIAGE_END_TIDAL_CO2_IN_PEDIATRIC_TRAUMA__A.1652.aspx
[23] Campion, E. M., Cralley, A., Robinson, C., Sauaia, A., Pieracci, F. M., Lawless, R. A., Platnick, B., Robinson, J., Edwards, D., McVaney, K., Moore, E. E., Cohen, M. J., Coleman, J. J., Fox, C., & Burlew, C. C. (2021). Prehospital end-tidal carbon dioxide predicts massive transfusion and death following trauma. Journal of Trauma and Acute Care Surgery, 89(4), 703-707. https://doi.org/10.1097/ta.0000000000002846
[24] Childress, K., Arnold, K., Hunter, C., Ralls, G., Papa, L., & Silvestri, S. (2018). Prehospital end-tidal carbon dioxide predicts mortality in trauma patients. Prehospital Emergency Care, 22(2), 170-174. https://doi.org/10.1080/10903127.2017.1356409
[25] Spaite, D. W., Bobrow, B. J., Keim, S. M., Barnhart, B., Chikani, V., Gaither, J. B., Sherrill, D., Denninghoff, K. R., Mullins, T., Adelson, D., Rice, A. D., Viscusi, C., & Hu, C. (2019). Association of statewide implementation of the prehospital traumatic brain injury treatment guidelines with patient survival following traumatic brain injury: The excellence in prehospital injury care (EPIC) study. JAMA Surgery, 154(7). https://doi.org/10.1001/jamasurg.2019.1152
[26] Baez, A. A., Qasim, Z., Wilcox, S., Weir, W. B., Loeffler, P., Golden, B. M., Schwartz, D., & Levy, M. (2022). Prehospital mechanical ventilation: An NAEMSP position statement and resource document. Prehospital Emergency Care, 26(1), 88-95. https://doi.org/10.1080/10903127.2021.1994676
[27] Diabetes Library. (n.d.). Pathophysiology of diabetic ketoacidosis. https://diabeteslibrary.org/pathophysiology-of-diabetic-ketoacidosis/
[28] Diabetes Talk. (2018, March 31). Metabolic acidosis compensation mechanism. https://diabetestalk.net/ketosis/metabolic-acidosis-compensation-mechanism
[29] Hunter, C. L., Silvestri, S., Ralls, G., & Papa, L. (2015). Prehospital end-tidal carbon dioxide differentiates between cardiac and obstructive causes of dyspnoea. Emergency Medicine Journal, 32(6), 453-456. https://doi.org/10.1136/emermed-2013-203405
[30] Hemnes, A. R., Newman, A. L., Rosenbaum, B., Barrett, T. W., Zhou, C., Rice, T. W., & Newman, J. H. (2010). Bedside end-tidal CO2 tension as a screening tool to exclude pulmonary embolism. European Respiratory Journal, 35, 735-741. https://doi.org/10.1183/09031936.00084709 [31] Riaz, I., & Jacob, B. (2014). Pulmonary embolism in Bradford, UK: Role of end-tidal CO2 as a screening tool. Clinical Medicine Journal, 14(2), 128-133. https://doi.org/10.7861/clinmedicine.14-2-129

Jonathan Mohnkern, BS, FP-C, CP-C, NRP, has worked in the EMS field for the past eight years with a background in rural, suburban, and urban settings. He currently operates as a 911 and transport paramedic in Upstate, NY. Jon holds a bachelor’s degree in biology and psychology, has experience in EMS management and tactical medicine, and is a current medical non-commissioned officer in the New York Army National Guard. Jon is currently in medical school as a first-year medical student and is passionate about critical care, pre-hospital medicine, and EMS education.
