Beating The Odds
In the dynamic landscape of cardiac care, Left Ventricular Assist Devices (LVADs) stand out as a beacon of hope and innovation. For patients grappling with advanced heart failure, where traditional medications and lifestyle adjustments fall short, LVADs offer a lifeline, bridging the gap between illness and a chance at extended life. These sophisticated devices are more than just mechanical aides; they are the culmination of years of medical advancement, embodying a commitment to enhancing and prolonging life. As we explore the world of LVADs, from their intricate design to their life-changing impact, we embark on a journey that intertwines cutting-edge technology with the core of human resilience and perseverance in the face of heart disease.
The firstline approach to a patient in heart failure is, of course, medication. Pharmacological treatment includes ACE inhibitors and ARBs, beta-blockers, diuretics, aldosterone antagonists, digitalis preparations, SGLT2 inhibitors, and hydralazine and nitrates. While these medications can significantly improve symptoms and ejection fraction for many patients, not all patients respond adequately to medical therapy alone. In cases of severely crippled hearts, a heart transplant is often the ultimate destination, but since spare hearts aren’t readily available there is a good amount of waiting and support needed until the patient reaches that destination.
LVADs have emerged as a beacon of hope for many patients whose heart needs more assistance. At their core, LVADs can be likened to a support system for a failing heart. Just as a garden with a failing watering system might rely on a supplemental water supply, an LVAD provides crucial support to a heart that’s struggling to pump blood effectively.
In heart failure, the heart’s ability to pump effectively is compromised. The left ventricle may become weak and unable to contract forcefully enough to maintain adequate blood flow. That brings up an important principle, or rather, a law of the heart. Starling’s Law of the Heart is a fundamental principle in cardiovascular physiology. It describes how the heart automatically adjusts its pumping function in response to changes in the volume of blood filling the heart (known as preload). The law states that the force of the heart’s contraction is directly proportional to the initial length of the cardiac muscle fibers at the end of diastole (when the heart is filled with blood). In simpler terms, this means that the more the heart is filled with blood during diastole, the more forcefully it will contract during systole.
Here’s a breakdown of how Starling’s Law works:
- Increased Preload: When more blood returns to the heart (increased preload), the ventricular muscle fibers stretch further.
- Enhanced Contractility: This stretching leads to a more forceful contraction of the heart muscle. Essentially, the heart pumps out more blood in response to receiving more blood.
- Optimized Stroke Volume: As a result, the heart’s stroke volume increases. This helps to maintain an equilibrium between the blood returning to the heart and the blood pumped out to the body and lungs.
Increased Preload
Heart muscle is stretched by increased blood return.
Enhanced Contractility
Stronger contractions of the heart muscles.
Optimized Stroke Volume
The heart pumps out larger volumes of blood to the body.
This relationship holds true up to a certain point. If the heart muscle is overstretched under the wrong conditions, as can happen in certain types of heart failure, the force of contraction may actually start to decrease, and the EF can worsen. Therefore, while the initial response to increased stretching (preload) is a stronger contraction and improved EF, this can become counterproductive if the stretching is excessive. This is a key consideration in the management of heart conditions, particularly Heart Failure with Reduced Ejection Fraction (HFrEF), also known as systolic heart failure. This type of heart failure occurs when the heart muscle weakens and the left ventricle can’t contract vigorously, leading to a reduced ejection fraction (less than 40%). In this case, while the heart is continuing to fill with the same amount of blood as it would when healthy, it simply can not compress and squeeze the blood out with any sort of efficiency.
Why do medications fail to help?
Medication can fail, or be less effective, in cases of advanced heart failure with reduced ejection fraction (HFrEF) for several reasons:
- Severity of Heart Damage: In advanced stages of heart failure, the heart muscle may be significantly weakened or damaged. Medications can help manage symptoms and slow disease progression, but they may not be able to fully compensate for the loss of heart function in severe cases.
- Progressive Disease Nature: Heart failure is often a progressive condition. Over time, despite medication, the heart can continue to weaken or become more dilated. This progression can reach a point where medications alone are insufficient to maintain heart function and quality of life.
- Remodeling of the Heart: Chronic heart failure can lead to changes in the size, shape, and function of the heart (known as remodeling). This remodeling can affect how effectively the heart responds to medications. For example, an enlarged and overstretched heart may not respond well to medications that would typically increase the strength of heart contractions.
- Comorbidities: Patients with heart failure often have other health issues (comorbidities) such as diabetes, kidney disease, or high blood pressure. These conditions can complicate the management of heart failure, making it harder for medications to be effective.
- Medication Tolerance and Side Effects: Over time, some patients may develop tolerance to heart failure medications, reducing their effectiveness. Additionally, side effects can limit the dosage or types of medications that a patient can tolerate.
- Adherence to Treatment: Patient adherence to medication regimens and lifestyle recommendations is crucial for managing heart failure. Non-adherence can lead to medication failure.
- Fluid Overload: In advanced heart failure, it becomes increasingly difficult to manage fluid overload, which can exacerbate heart failure symptoms and reduce the effectiveness of medications.
So then how do LVADs help?
Ok, so now what? Medications have failed, and there isn’t a healthy heart just laying around waiting to get swapped out with the sick one. Science suggests people without a heart are, in fact, incompatible with life. Continuous flow cardiac assist devices, such as Left Ventricular Assist Devices (LVADs), are designed to address this issue. Unlike the heart’s natural pumping action (the Starling’s Law of the Heart one that is broken), these devices provide a continuous flow of blood via a surgically implanted device that takes over some or most of the pumping function of the left ventricle. Blood is drawn from the left ventricle into the device and then propelled into the aorta. These devices, often referred to as a bridge to transplant or a destination therapy, have revolutionized the treatment of severe heart failure.
Quick video of how an LVAD is implanted and how it works INSIDE THE BODY
Isn’t that amazing? Here’s the thing… as a pre-hospital, or critical care transport medicine provider there is nothing you are going to be able to do with the INSIDE part of these devices. That’s the surgeon’s playground, so if you see any of these parts when you are doing a transport, it’s a bigger emergency than you think it is! However, it is important to understand the inside part, so you have a better understanding of the OUTSIDE part that you will most certainly interact in transport.
All the parts on the OUTSIDE OF THE BODY
An LVAD consists of several external components that are crucial for its operation. Understanding these components is essential if you are involved in critical care transport. One of the most important things to remember is that the patient and their family is usually far more knowledgeable about the use of the device than you are and that’s OK because the patient’s life literally dependent on the device. When they receive the device they also receive a lot of education about it. So, learn as much as you can, but also lean on their knowledge to help fill in the blanks.
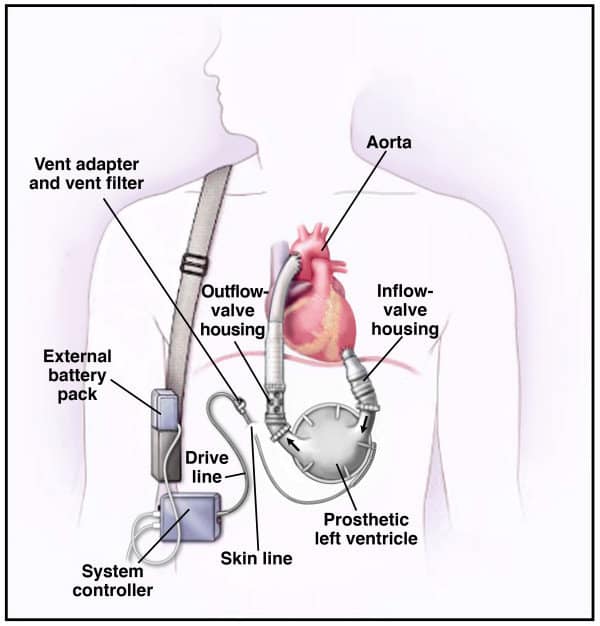
Each device is slightly different, but it’s important to get the basics down. Here’s a breakdown of the outside parts of an LVAD and how providers interact with them:
- Controller:
The controller is the ‘brain’ of the LVAD. It’s a small, portable computer that regulates the pump’s speed and function. It displays vital information such as battery life, pump speed, and alarm notifications. There will likely be a manual or quick-reference guide kept with the patient’s LVAD controller. This manual usually contains crucial information about the LVAD system, including how to operate the controller, interpret alarms, manage power sources, and troubleshoot common issues.- Emergency Reference: In emergency situations, healthcare providers, especially those unfamiliar with the specific model of LVAD, can quickly refer to the manual for guidance on how to respond to alarms or other issues with the device.
- Caregiver and First Responder Guidance: The manual serves as an immediate resource for caregivers or first responders who may need to assist the patient but are not intimately familiar with the workings of the device.
- Patient Safety: Having immediate access to the device manual enhances patient safety, ensuring that any issues can be addressed promptly and correctly.
- Consistency in Care: It provides a consistent source of information, which is particularly important when multiple healthcare providers are involved in the patient’s care.
- Transportation and Transfer of Care: During transport, whether it’s a routine appointment or an emergency situation, the manual can be invaluable in ensuring that the patient receives appropriate care when they are handed over to a new care team.
- Driveline:
The driveline is a cable that exits the patient’s body, usually at the abdomen, and connects the internal pump to the external controller. It transmits power and information between the pump and the controller. You should frequently assess that the driveline is secure and free from damage (especially during patient moves). - Power Source:
The power source for an LVAD can be batteries or a connection to an electrical outlet. Batteries are portable and used when the patient is mobile, while AC adapters are used for stationary power supply. You should check the battery levels frequently before and during transport. - Carrying Case:
This is a bag or case used to carry the controller and battery pack. It’s designed for convenience and safety, allowing patients to move around freely. While providers may not directly interact with the carrying case, they should ensure that it’s properly secured during transport and that it does not impede the patient’s comfort or the functionality of the device.
Managing the LVAD during transport
During transport of a patient with a Left Ventricular Assist Device (LVAD), the most common adjustments made to the device typically involve managing the power source and responding to alarms. It’s important to note that significant adjustments to the device’s settings (such as pump speed or flow rate) are usually done under the guidance of a specialized LVAD team and are not typically adjusted during transport unless in an emergency situation. Here are the common adjustments and considerations for transport providers:
- Power Source Management:
- Battery Changes: Ensure that the LVAD is connected to a reliable power source. This usually means checking the battery life before transport and having spare, fully charged batteries on hand. If a battery change is needed, you should know how to safely swap batteries without interrupting the device’s operation.
- AC Power: For longer transports, or if the patient is stationary for a period, switching to AC power might be necessary. You should understand how to safely switch from battery to AC power.
- Responding to Alarms:
- Alarm Interpretation: LVADs have various alarms for different issues like low battery, low flow, or high power usage. You should be familiar with the basic alarms and what they indicate. This is where the manuals come in handy!
- Initial Response: Providers should know the initial response to common alarms, such as checking connections, ensuring there are no kinks in the driveline, and checking the controller for error messages.
- Emergency Protocols: Have a clear understanding of the protocols for responding to critical alarms, including when to contact the LVAD team or initiate emergency procedures.
- Monitoring and Observation:
- Device Functionality: Regularly monitor the LVAD controller for any changes in readings or unexpected alerts.
- Patient Assessment: Continuously assess the patient’s condition, watching for signs of distress or changes in their clinical status.
- Environmental Considerations:
- Temperature and Weather: Ensure the device and patient are protected from extreme temperatures and kept dry, as extreme conditions can affect device function.
- Communication with LVAD Team:
- Pre-Transport Coordination: Ideally, discuss any specific concerns or instructions with the patient’s LVAD team prior to transport.
- During Transport: Have the means to contact the LVAD team for guidance if unusual situations or device issues arise.
Remember, the primary role of the critical care transport medicine provider in the transport of patients with LVADs is to ENSURE THE PATIENT’S SAFETY AND STABILITY, not to manage the LVAD settings in-depth. Any significant concerns or device malfunctions should be addressed in coordination with the patient’s LVAD team. The focus should be on maintaining the current settings, ensuring power supply continuity, and responding to basic alarms or issues.
Each LVAD represents more than just a triumph of technology; it symbolizes hope, a renewed chance at life, and the profound impact of compassion combined with human ingenuity. You are not just transporting a patient; you are carrying hope, sustaining dreams, and bridging the gap between despair and life. The knowledge you gain and the care you provide makes all the difference in providing better outcomes and more tomorrows for your patients.
