Undifferentiated Shock: A Pre-hospital Approach
Shock is the final common pathway before death. No matter what the etiology or insult to the human body, we all will enter into a state of shock that reduces oxygen delivery to the point that cells die, then tissues die, organs become dysfunctional, then organ systems fail, and finally the whole machinery of human life is completely unhinged… in some cases, irreversibly.
In the hospital, although to little effect on the outcome, there are plentiful resources and departments designed to assist a resuscitationist with the work of stabilizing, differentiating, and treating a patient in shock. Those resources do not exist in the prehospital environment, and despite the technological advances that exist to approximate the level of care rendered inside a hospital, the prehospital and transport environments often are lacking a system robust enough to ease the burden of the resuscitationist in the management of shock.
What are we to do? It is my belief that in this environment and context, the prehospital provider must rely on accurate mental models and functional heuristics to make the best decisions on how to best stabilize, differentiate, and treat these patients who are seemingly so close to the edge that we may not get them back.
Shock: A Way
The stabilization and resuscitation of a patient in shock, regardless of etiology, relies on the proper approach and mental model for success. In 2023 there is no shortage of internet resources that provide us with some great mnemonics and cognitive devices that are designed to help us remember the main etiologies of shock:
- Cardiogenic
- Hypovolemic
- Distributive
- Obstructive
What we lack is a great mental model for working completely through the patient’s physical exam and history to arrive at the culprit issue causing the shock state. Sometimes to prime the mind for the differentiation of these shock states, we attempt to commit these complicated collections of signs and symptoms to memory and hope to trip over enough information so as to be able to assign the patient to the proper category. It may look something like this:
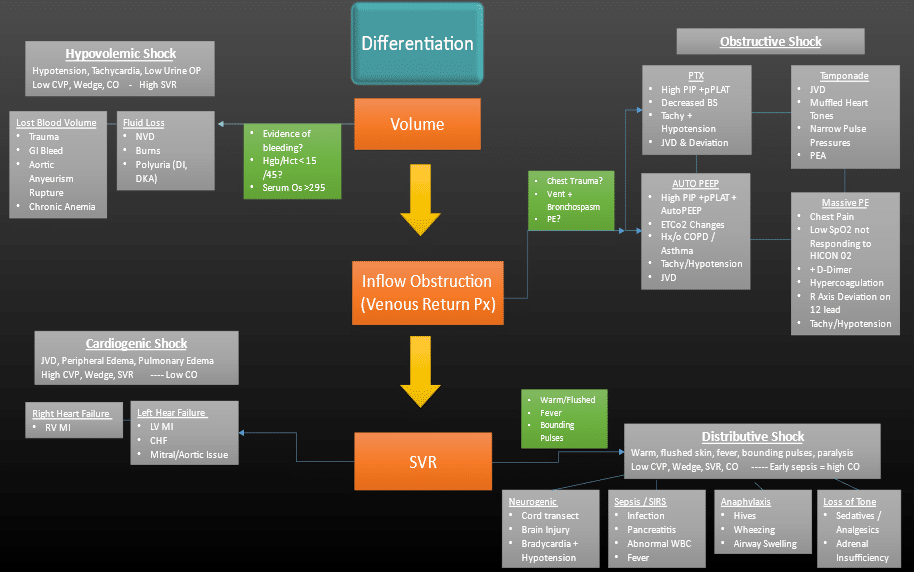
This seems like a lot of information to try to access in the heat of the moment while under duress. Perhaps there is a different way to approach this:
- Stabilize the ABCs to optimize oxygen delivery.
- Differentiate what you are seeing so that you know what the patient is suffering from.
- Resuscitate, aggressively, the shock etiology you have discovered.
- Optimize your strategy for the best possible outcome.
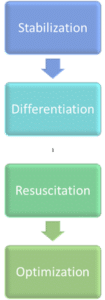
Stabilization
Stabilization is focused on the successful management of the airway, selecting a strategy of mechanical ventilation that lends itself to successful resuscitation and not one that works against you, and finally ensuring that vascular access is obtained, functional, and that the first line medications and treatments to stabilize blood pressure have been initiated (volume, vasopressors, etc.). Some attention also needs to be given to the patient’s ability to carry oxygen (e.g. H&H/hemoglobin) to ensure that our resuscitation strategy optimizes volume status without causing hemodilution. Remember, this is simply stabilization, not normalization. The focus is putting interventions in place that begin moving the patient in the right direction, prioritizing the ABCs before moving on to an in-depth investigation of the underlying cause.

Differentiation and Resuscitation
Differentiation and Resuscitation should be thought of as a cycle. We investigate a little, differentiate what we think the problem is, and then resuscitate. It requires that we constantly ask ourselves a few questions:
- “What can I fix?”
- “Where can I/ should I look?”
- “Did the intervention work?”
- “Do I need to escalate it?”
Amal Mattu does a fantastic talk on ways to avoid errors in the management of shock (https://youtu.be/4U0K1qVcLlA), and I have adopted his thought process into my own resuscitation strategy. Instead of waiting for the patient to check enough boxes to classify them into a particular shock diagnosis (an approach that will likely lead you to miss a diagnosis), assume that a shock state is there and go look for it. This thought process coupled with a cycle of resuscitation and differentiation can prove to be a more effective approach to the undifferentiated shock patent.
I have modified Dr. Mattu’s approach to something I can replicate in the prehospital environment:
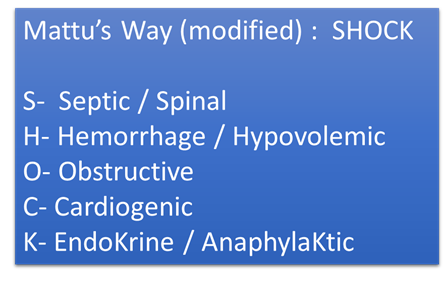
This should not be looked at as a list of things to consider, but rather a list of things to go investigate, find or not, and resuscitate/correct as you move through your clinical course with the patient. The thought process is, for example, assume that the patient is in obstructive shock until you can rule out a tension pneumothorax, PE, etc. Then move on to looking for cardiogenic shock and so on.
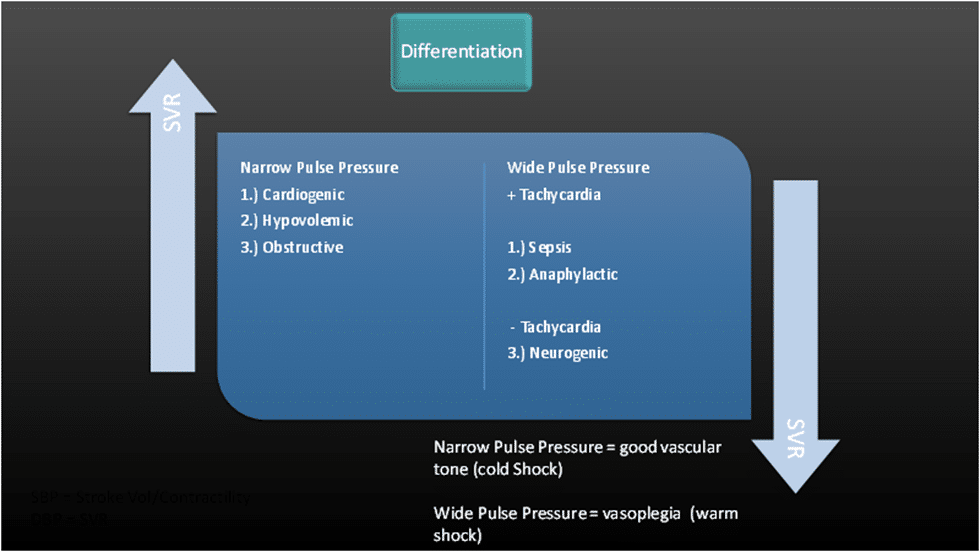
In some cases, there may not be time to confirm whether a particular cause of shock it present. Perhaps there is a faster way? If you can get a MAP, pulse pressure, and a heart rate, you can identify the culprit shock state and more accurately/adequately resuscitate your patient.
A quick primer on pulse pressure. Pulse pressure (PP) is the difference between the systolic blood pressure and the diastolic blood pressure. It is described as either wide or narrow and is a useful tool in the differentiation of various shock states when evaluated in concert with the patient’s heart rate.
Pulse pressure makes a lot more sense when we look at what the systolic and diastolic pressures are telling us. Traditionally, we are taught that the systolic blood pressure (SBP) is the contraction and the diastolic blood pressure (DBP) is “relaxation or filling.” In actuality, they can be extrapolated to be indicators of left ventricular function (SBP) and vascular tone (DBP). We then look at the MAP as a measure of how well the system is working overall. Our numbers suddenly mean a lot more to us. We will find one of the following:
- Intact cardiac function with poor vascular tone
- Poor cardiac function with good vascular tone
- Poor cardiac function and poor vascular tone
Narrow Pulse Pressure:
A narrow pulse pressure means that the systolic and diastolic blood pressures are close together. What it is telling us is that there is not a problem with the vasculature and that vascular tone is intact for the most part, but the problem lies in the LV. When coupled with tachycardia we can begin to rule in or rule out: cardiogenic shock, hypovolemic shock, and/or obstructive shock. In each of these the vascular system is intact and functioning, but there is either a preload, afterload, or contractility problem that is inhibiting the function of the LV, thereby manifesting as a low SBP.
Wide Pulse Pressure + Tachycardia:
A wide pulse pressure (when the systolic and diastolic are farther apart) is telling us that the LV is functioning reasonably well and that there is a problem with the vasculature. This should indicate a septic shock or an anaphylactic shock, both shock states where the cardiac function is intact (although not unaffected) and vasodilation or vaso-plegia are the culprits.
Wide Pulse Pressure – Tachycardia:
There is only one shock state that typically manifests as hypotension and normal HR or bradycardia: neurogenic shock. The LV is functioning fine, but the nervous system has been disrupted and cannot communicate with the vascular system.
When evaluating patients in shock, the systolic blood pressure alone is not enough information to develop the most appropriate resuscitation strategy. Literally the only thing it is telling us is that the patient is hypotensive, not why. Prehospital providers should then look for secondary indicators of poor perfusion to confirm their impression of shock, e.g., pulse oximetry that is persistently low with poor pleth wave or EtCO2 that is persistently in the 20s.
Optimization
After the initial stabilization and differentiation of the patient, there should be an evaluation for what is the most optimal way to manage the patient moving forward. This may be evaluating for the need to deescalate some of your initial stabilization measures, or adding a second line agent to improve their hemodynamics. It may be looking at your ventilator settings and ensuring that they are optimized for the patient’s needs, basing titrations on data from blood gases from that point forward.
There are many strategies and approaches to optimizing the patient for transport and movement to the final destination. Those strategies should be oriented toward balance. There is a delicate balancing act that must take place at this point to ensure that intervention A does not have an overly negative impact on measure B, etc. Maintain awareness of cardiorespiratory interactions when a patient is receiving ventilatory support and the potential for negative hemodynamic effects that may be present while receiving positive pressure ventilation. Keep the fundamentals of human hemodynamics in the top of your mind (e.g., things like Poisuellie’s Law).
Close Out
Stabilizing, differentiating, and resuscitating a critically ill patient is no small task and one that is fraught with pitfalls and danger. It is essential to take a deliberate but step-wise approach to these patients. They must be stabilized before they can be studied and differentiated, and then we must take the time to revisit our strategy and interventions to ensure they are the best for the conditions we have identified. Keep things as simple as possible and maintain focus on the parameters that give you the most useful information that you can use to base decisions for decision making ( e.g., focus on MAP or pulse pressure rather than a systolic blood pressure alone).
Keep it basic. Keep it simple.

Cody Winniford, BA, EMT-P, CCP-C, FP-C
Cody has been in EMS for 18 years, serving in both military and civilian settings. His professional experiences include serving as an educator for initial paramedic instruction programs, clinical manager, EMS operations manager, and EMS Operations Director. He is currently serving as a flight paramedic with PHI Air Medical and volunteers for the education committee for the ICAPP.
