The Remarkable Versatility of Ketamine: A Review of Pre-Hospital and Critical Care Use
Ketamine is a non-barbiturate dissociative anesthetic originally synthesized in the 1960s. In lower doses, ketamine acts as a potent analgesic, causing it to be adapted to manage pain during the Vietnam War.(1,2) Ketamine acts as an N-methyl-D-aspartate (NMDA) receptor antagonist. NMDA receptors are a type of glutamate receptor, which bind with glutamate, the principal excitatory neurotransmitter in the central nervous system. Clinically, glutamate plays a significant role in numerous pathways, including learning and memory, pain, and sleep-wake cycles, allowing ketamine to serve as a versatile pharmaceutical agent.(3) Additionally, glutamate plays a role in seizures and excitotoxicity after nervous system injury. This article will review potential mechanisms and evidence surrounding ketamine in pre-hospital and critical care settings.
Pain Management
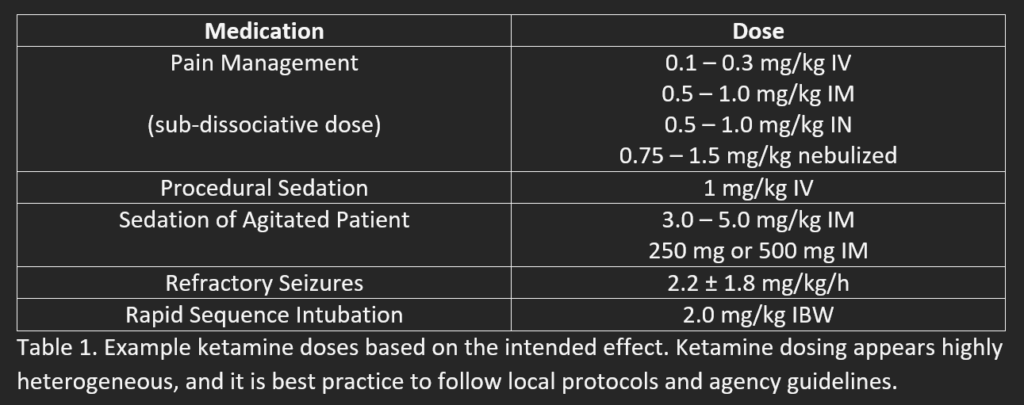
The onset of action of ketamine is 30 seconds intravenous and approximately 4 minutes intramuscular. (2) Ketamine acts on the sympathetic nervous system to stimulate cardiovascular and respiratory function, which reduces the risk of respiratory depression that is sometimes seen with opioids. (2) Ketamine is also believed to maintain pharyngeal and laryngeal reflexes. (2) These considerations, in addition to the ongoing opioid epidemic, have made ketamine an attractive medication in clinical settings.
In reviewing available evidence on ketamine, it is first necessary to acknowledge that pain management and associated documentation in the pre-hospital setting is largely insufficient in some EMS systems.(4,5). A small amount of evidence exists that ketamine administration is more effective in managing acute pain than opioids. (6) However, the validity of these studies is low and requires further investigation. Recent evidence suggests that ketamine and opioids are likely similar in their ability to manage acute pain.(5,7,8,9,10)
Opioids are more commonly likely to cause nausea, vomiting, and respiratory depression in comparison to ketamine. (6) On the contrary, ketamine is found to cause more dizziness and feelings of unreality. (2,11,12) Overall, the adverse effects of ketamine for pain management are low, transient, and often do not require intervention. (11) An exception to this is the emergence phenomenon, which occurs in a small population of patients that receive ketamine. (2,13) The emergence phenomenon may have different presentations but is commonly described as severe agitation, hyperactivity, altered mental status, and schizophrenia-like features. (2,13) Treatment for this condition includes benzodiazepines. (2) Due to the adverse reactions, some fear that ketamine may lengthen hospital stays, but this has not been shown in most clinical studies. (13)
Ketamine is a primary analgesic agent in military medicine for adult and pediatric populations.(14,15,16) Currently, opioids are likely to remain the first-line therapy for acute pain in most civilian clinical settings. However, ketamine may play a role in particular circumstances. For example, individuals may have allergies or previous negative experiences with opioid medications. (5,7) Ketamine is also helpful for patients with opioid tolerance, a history of opioid abuse, or who are taking Suboxone. (7,17) In refractory pain, ketamine can be safely combined with nitric oxide and opioids to provide additional comfort. (11) Studies have illustrated that mixing opioids and ketamine is likely more effective and quicker in relieving pain than re-administering opioids. (9,10,17) Ketamine is an excellent adjunct for traditionally challenging conditions, such as refractory pain related to sickle cell crisis. (18,19) Lastly, ketamine is effective in IV, IM, IN, and nebulized routes, which allows providers diverse methods to provide pain relief. (5-12,17,19)
Chronic Pain
EMS providers may witness patients that use ketamine infusions for chronic pain. Various studies have connected chronic pain to loss of descending pathway inhibition of pain signals, immune cell activation, the release of inflammatory cytokines, neuroplasticity, and upregulated NMDA receptor expression and phosphorylation. (1) Ketamine is believed to reduce chronic pain by altering these mechanisms. Another method by which ketamine may reduce chronic pain is by binding to muscarinic acetylcholine receptors or changing serotonergic signaling. (1) Ketamine appears to help manage chronic pain, but we currently have limited data on long-term effects. (20) The ROCKet trial is being conducted, taking a closer look at ketamine use in chronic pain. Some complications that have been seen include pathological sympathetic stimulation, hepatotoxicity, cystitis, behavioral changes, and dependency. (20)
Procedural Sedation Analgesia
Procedural sedation analgesia (PSA) is administering medications to reduce a patient’s discomfort during a traditionally painful intervention. PSA procedures may be utilized during limb realignment, electrical cardioversion, lumbar puncture, and many other conditions that may be uncomfortable for the patient. (21,22) No single combination of PSA medications applies to every patient due to their underlying medical conditions, ongoing pathology, and current level of pain or anxiety. Ideally, PSA medications cause transient dissociation and pain relief to patients but maintain cardiovascular and respiratory functioning. (21,22) Based on this definition, ketamine is an effective medication for procedural sedation. Other common medications for PSA include benzodiazepines, opiates, propofol, remifentanil, alfentanil, dexmedetomidine, etomidate, and nitrous oxide. Studies illustrate that ketamine is the most common pre-hospital PSA agent utilized, and it appears to reduce painful experiences more than opioid use alone.(23) Further, combining ketamine with smaller doses of other agents, such as propofol, decreases the incidence of respiratory depression and other complications than propofol alone. (24) It is essential to acknowledge that despite the safety profile of ketamine as a procedural sedation agent, clinicians should anticipate the need to provide airway and respiratory interventions after administration. (22)
Sedation for Patient/Crew Safety
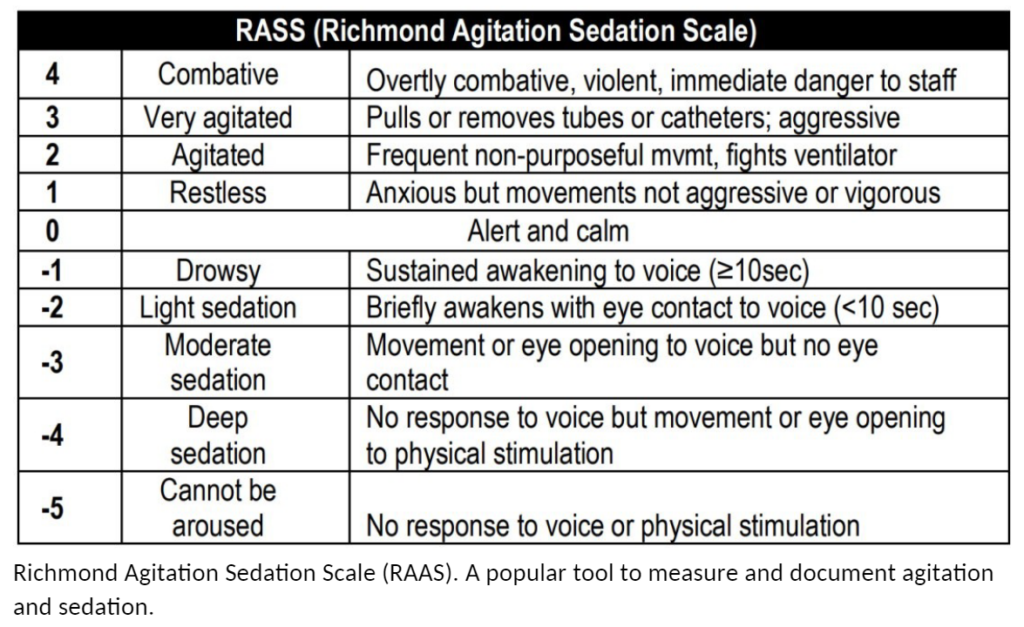
Some patients present to EMS crews with signs of severe agitation that make them a threat to themselves, bystanders, and medical personnel. First, it is crucial to appreciate that verbal de-escalation is the primary intervention. However, this is not always possible; in some cases, there is no way to assess and transport the patient safely. Common medications used in sedation include benzodiazepines, antipsychotics (ex: haloperidol), and ketamine. (25) Each medication has trade-offs between adequate sedation and unique adverse effects. First, ketamine is frequently used in this scenario due to its rapid onset, reliable ability to produce a dissociated state, wide therapeutic window, and limited suppression of airway reflexes. (26,27) The downsides of ketamine include hypersalivation, laryngospasm, emergence reactions, and a higher incidence of intubation. (26-31)
Benzodiazepines are widely available to EMS providers and have a relatively wide safety profile. (26) However, they have a slower onset with significant variability in dose response, requiring more active titration and unpredictable effects. (26) Further, benzodiazepines are known to cause respiratory depression and hypotension at high doses.
Lastly, haloperidol antagonizes dopamine receptors and is an attractive agent for treating hyperdopaminergic causes of agitation. (26) However, haloperidol illustrates a slow onset and has the potential to cause extrapyramidal reactions, prolonged QT, seizures, and torsades de pointes(25-27,29
Ketamine appears to provide the fastest route to adequate sedation but illustrates the highest rate of adverse effects. A recent meta-analysis indicates that the intubation rate after ketamine administration is lower than we once believed but is still more common than the combination of versed and haloperidol. (29) In severe agitation where imminent life threats exist, rapid onset and dissociation of ketamine probably outweigh the potential adverse effects. (25,30) It is imperative that clinicians anticipate these complications, have airway/ventilatory equipment prepared, and are competent in airway management.
Sedation in Mechanically-Ventilated Patients
Mechanically-ventilated patients frequently receive continuous sedation with fentanyl, propofol, midazolam, and dexmedetomidine. (32) A recent meta-analysis illustrates the increasing use of ketamine as an adjunct to these medications. (32) Recent evidence indicates that ketamine may be sedative-sparing by reducing the amount of propofol required for continuous sedation. (32) Therefore, ketamine may be especially helpful in hemodynamically unstable patients as vital signs remain relatively unchanged with ketamine compared to propofol. (33)
Ketamine also appears to reduce the consumption of opioids in mechanically-ventilated patients. (34) In addition, ketamine does not appear to show any significant difference in the length of mechanical ventilation, length of stay, intracranial pressure, or mortality. (34) Further studies are required to determine the prevalence of psychomimetic adverse effects (delirium, hallucinations) that are challenging to detect and poorly reported. (32)
Refractory Seizures
Status epilepticus refers to a continuous seizure lasting > 5 minutes or multiple episodes without a return to normal mental status. (35) The general approach to these patients includes immediate benzodiazepine administration, antiepileptic administration (Keppra), and evaluation for reversible causes. (35, 36) For example, pathologies such as hypoglycemia, thiamine deficiency, eclampsia, hyponatremia, and increased intracranial pressure require additional treatments to terminate and avoid continual seizures. (35,36)
Benzodiazepines act on GABA-A receptors, which interact with GABA, a major inhibitory neurotransmitter in the central nervous system. Benzodiazepines cause central nervous system depression by enhancing the opening of inhibitory chloride channels. (37) Rapid treatment of status epilepticus is critical as the efficacy of benzodiazepines appears to decrease over time due to GABA receptor downregulation. (37)
Sedative medications such as ketamine and propofol become an option in severe circumstances when seizures are refractory to benzodiazepines and traditional antiepileptics. (36,38,39) As discussed previously, ketamine is an antagonist to NMDA receptors, which may have synergist effects with benzodiazepines acting together to stop seizures. Early evidence indicates that continuous infusions of ketamine reduce the burden of seizures without significant adverse effects. (38,39)
Adjunct to Non-Invasive Ventilation
Non-invasive ventilation (NIV) is frequently applied in the form of continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP). NIV is a necessary treatment to manage respiratory distress, which reduces the need for endotracheal intubation. NIV is effective in respiratory distress by reducing the work of breathing, improving alveolar recruitment, decreasing V/Q mismatch, and improving alveolar gas exchange and removal of carbon dioxide. (40)
Hypoxic patients with respiratory distress may not tolerate the masks involved in NIV due to anxiety or altered mental status. Efforts should be made to improve mask tolerance via verbal coaching, increasing oxygen flow, or changing ventilator settings, such as reducing rise time. Ketamine is an agent that can be used to reduce anxiety and cause mild sedation to improve patient tolerance if the previous interventions are not enough. (40-42) Ketamine is especially attractive for asthma and chronic obstructive pulmonary disease as it acts as a bronchodilator. (43) A review of multiple studies indicates that ketamine can effectively reduce bronchospasm in refractory status asthmatics. (43) In addition, case studies exist that illustrate the ability of ketamine to improve bronchospasm in pediatric asthma exacerbation, anaphylaxis, and even organophosphate poisoning. (44,45,46)
Airway Management
Throughout this article, we have discussed the risk of intubation as an adverse effect of ketamine administration. However, ketamine is also used to do just that – as a popular induction agent in rapid sequence intubation (RSI). Ketamine theoretically maintains hemodynamics (47), but it can still cause hypotension, especially when the shock index is > 0.9 (shock index = heart rate / systolic blood pressure). There appears to be no significant difference in hypotension, mortality, or first-pass success when comparing ketamine to etomidate. (47) It was once believed that ketamine should be avoided in cases of increased intracranial pressure, intraocular pressure, or psychiatric conditions, but current evidence does not demonstrate clinical significance. (47)
Ketamine is frequently used during delayed sequence intubation (DSI), where medications are provided to cause dissociative sedation while maintaining airway reflexes. This allows effective preoxygenation before administering a paralytic agent. (48). Sometimes, the patients respond exceptionally well to non-invasive positive pressure ventilation and avoid intubation. (48)
Psychological Treatment
Without going too in-depth, ketamine is also used for conditions such as post-traumatic stress disorder, refractory anxiety, and major depressive disorder, poorly managed with standard treatment. (49-51) Common acute side effects after ketamine treatment include dizziness, blurry vision, headache, feelings of dissociation, and nausea/vomiting. (49,50,51) In rare cases, sympathetic nervous system activation by ketamine may cause clinically significant tachycardia or hypertension. (49)
Conclusion
Ketamine is a versatile drug that can fit many different roles in your career as a clinician. Ketamine is primarily used for RSI/DSI, sedation, and pain management. Further, it is becoming more popular in treating refractory seizures, chronic pain, and psychological disorders and improving NIV mask toleration.
Summary
- Ketamine acts primarily as an antagonist of N-methyl-D-aspartate receptors (NMDA receptors), which binds glutamate, the primary excitatory neurotransmitter in the CNS.(1,2)
- NMDA receptors have many isoforms with different pharmacologic properties, allowing ketamine to act as a versatile therapeutic agent. (2)
- The primary metabolism of ketamine occurs in the liver. (2)
- Ketamine is an effective analgesic that can be used in isolation or in combination with opioids. Instances of when to use ketamine may include opioid allergy, opioid tolerance, opioid abuse, Suboxone prescription, severe fear of opioids, or pain refractory to standard opioid management. (5-20)
- Ketamine can be administered via IV, IM, IN, or nebulized routes for analgesia. (5-20)
- Ketamine is an effective agent for procedural sedation as it provides dissociative and analgesic effects without typically losing airway reflexes or respiratory function. (21-24)
- Common medications used to sedate severely agitated patients include benzodiazepines, antipsychotics (haloperidol), and ketamine. Ketamine is an attractive sedative for these patients due to its rapid onset, IM administration, and theoretical protection of airway reflexes and ventilatory status. However, evidence suggests a trade-off between ketamine vs. other sedative agents: it provides adequate sedation quicker, but it poses a higher risk of adverse effects. In the situation of genuine severe agitation, the benefits of quick sedation may outweigh the negative effects. (25-31)
- Ketamine may be a helpful adjunct in continual sedation in mechanically-ventilated patients by reducing the amount of sedatives and opiates while maintaining cardiac output. (32-34)
- Status epilepticus is a medical emergency that requires immediate treatment with benzodiazepines and anticonvulsants. As the seizure continues, patients appear less responsive to benzodiazepines and may require numerous anticonvulsants. Preliminary evidence illustrates the efficacy of ketamine as an anticonvulsant in refractory status epilepticus. (35-39)
- Ketamine may improve mask toleration during non-invasive ventilation with CPAP or BiPAP while also providing bronchodilation in patients with bronchospasm. (41-46)
- Ketamine is frequently used in rapid sequence intubation and delayed sequence intubation. It usually does not affect hemodynamics but may cause hypotension when the shock index is high (> 0.9). (47)
- There is limited evidence that ketamine use causes worse outcomes in patients with increased intracranial pressure, intraocular pressure, or psychiatric conditions. (47)
- Ketamine is gaining popularity in treating anxiety disorders, PTSD, and major depressive disorders. (49-51)
- While ketamine appears to have a safe profile, it is crucial that dosing is correct; it is beneficial for agencies to implement safety guidelines regarding the administration of controlled substances – review protocol, create a table for dosing to avoid calculation errors, dose review with a partner, EtCO2 placement.
References
- Iacobucci GJ, Visnjevac O, Pourafkari L, Nader ND. Ketamine: An update on cellular and subcellular mechanisms with implications for clinical practice. Pain Physician. 2017;20(2):285-301. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28158165/
- Rosenbaum SB, Gupta V, Palacios JL. Ketamine. StatPearls Publishing; 2022. Accessed August 10, 2022. https://pubmed.ncbi.nlm.nih.gov/29262083/
- Cleveland Clinic medical professionals. Glutamate. Clevelandclinic.org. Published April 25, 2022. Accessed December 26, 2022. https://my.clevelandclinic.org/health/articles/22839-glutamate
- Gerhardt RT, Reeves PT, Kotwal RS, Mabry RL, Robinson JB, Butler F. Analysis of prehospital documentation of injury-related pain assessment and analgesic administration on the contemporary battlefield. Prehospital Emergency Care. 2016;20(1):37-44. https://doi.org/10.3109/10903127.2015.1051683
- Lindbeck G et al. Evidence-based guidelines for prehospital pain management: Recommendations. Prehospital Emergency Care; 2022:1-10. https://doi.org/10.1080/10903127.2021.2018073
- Bronsky ES, Koola C, Orlando A, Redmond D, D’Huyvetter C, Sieracki H, Tanner A 2nd, Fowler R, Mains C, Bar-Or D. Intravenous low-dose ketamine provides greater pain control compared to fentanyl in a civilian prehospital trauma system: A propensity matched analysis. 2019;23(1):1-8. https://doi.org/10.1080/10903127.2018.1469704
- Frey TM, Florin TA, Caruso M, Zhang N, Zhang Y, Mittiga MR. Effect of intranasal ketamine vs. fentanyl on pain reduction for extremity injuries in children: The PRIME randomized clinical trial. JAMA Pediatrics. 2019;173(2):140-146. https://doi.org/10.1001/jamapediatrics.2018.4582
- Sin B, Tatunchak T, Paryavi M, Olivo M, Mian U, Ruiz J, Shah B, de Souza S. The use of ketamine for acute treatment of pain: A randomized, double-blind, placebo-controlled trial. The Journal of Emergency Medicine. 2017;52(5):601-608. https://doi.org/10.1016/j.jemermed.2016.12.039
- Sobieraj DM, Martinez BK, Miao B, Cicero MX, Kamin RA, Hernandez AV, Coleman CI, Baker WL. Comparative effectiveness of analgesics to reduce acute pain in the prehospital setting. Prehospital Emergency Care. 2020;24(2):163-174. https://doi.org/10.1080/10903127.2019.1657213
- Yousefifard M, Askarian-Amiri S, Rafiei Alavi SN, Sadeghi M, Saberian P, Baratloo A, Talebian MT. The efficacy of ketamine administration in prehospital pain management of trauma patients; A systematic review and meta-analysis. Archives of Academic Emergency Medicine. 2019;8(1). https://pubmed.ncbi.nlm.nih.gov/32021982/
- Bowers KJ, McAllister KB, Ray M, Heitz C. Ketamine as an adjunct to opioids for acute pain in the emergency department: A randomized controlled trial. Academic Emergency Medicine. 2017;24(6):676-685. https://doi.org/10.1111/acem.13172
- Andolfatto G, Innes K, Dick W, Jenneson S, Willman E, Stenstrom R, Zed PJ, Benoit G. Prehospital analgesia with intranasal ketamine (PAIN-K): A randomized double-blind trial in adults. Annals of Emergency Medicine. 2019;74(2):241-250.
- Robinson EJ, Watanabe BL, Brown LH. Ketamine for prehospital pain management does not prolong emergency department length of stay. Prehospital Emergency Care. 2021;25(6):753-760. https://doi.org/10.1080/10903127.2020.1819493
- Schauer SG, Mora AG, Maddry JK, Bebarta VS. Multicenter, prospective study of prehospital administration of analgesia in the U.S. combat theater of Afghanistan. Prehospital Emergency Care. 2017;21(6):744-749. https://doi.org/10.1080/10903127.2017.1335814
- Schauer SG, Arana AA, Naylor JF, Hill GJ, April MD. Prehospital analgesia for pediatric trauma patients in Iraq and Afghanistan. Prehospital Emergency Care. 2018;22(5):608-613. https://doi.org/10.1080/10903127.2018.1428839
- Schauer SG, Naylor JF, Maddry JK, Hinojosa-Laborde C, April MD. Trends in prehospital analgesia administration by US forces from 2007 through 2016. Prehospital Emergency Care. 2019;23(2):271-276. https://doi.org/10.1080/10903127.2018.1489022
- Morgan MM et al. Ketamine use in prehospital and hospital treatment of the acute trauma patient: A joint position statement. Prehospital Emergency Care. 2021;25(4):588-592. https://doi.org/10.1080/10903127.2020.1801920
- Hagedorn JM, Monico EC. Ketamine infusion for pain control in acute pediatric sickle cell painful crises. Prehospital Emergency Care. 2019;35(1):78-79. https://doi.org/10.1097/pec.0000000000000978
- Patrick C, Smith M, Rafique Z, Rogers Keene K, De La Rosa X. Nebulized ketamine for analgesia in the prehospital setting: A case series. Prehospital Emergency Care. 2022;1-6. https://doi.org/10.1080/10903127.2022.2099602
- Clark JD. Ketamine for chronic pain: Old drug new trick? Anesthesiology. 2020;133(1):13-15. https://doi.org/10.1097/aln.0000000000003342
- American College of Emergency Physicians. Procedural sedation in the emergency department. Published July 2017. Accessed December 27, 2022. https://www.acep.org/patient-care/policy-statements/procedural-sedation-in-the-emergency-department/
- Benzoni T, Cascella M. Procedural Sedation. StatPearls publishing; 2022. Accessed September 3, 2022. https://pubmed.ncbi.nlm.nih.gov/31869149/
- Galinski M et al. Procedural sedation and analgesia in trauma patients in an out-of-hospital emergency setting: A prospective multicenter observational study. Prehospital Emergency Care. 2018;22(4):497-505. https://doi.org/10.1080/10903127.2017.1413464
- Ghojazadeh M, Sanaie S, Paknezhad SP, Faghih SS, Soleimanpour H. Using ketamine and propofol for procedural sedation of adults in the emergency department: A systematic review and meta-analysis. Advanced Pharmaceutical Bulletin. 2019;9(1):5-11. https://doi.org/10.15171/apb.2019.002
- Barbic D, Andolfatto G, Grunau B, Scheuermeyer FX, Macewan B, Qian H, Wong H, Barbic SP, Honer WG. Rapid agitation control with ketamine in the emergency department: A blinded, randomized controlled trial. Annals of Emergency Medicine. 2021;78(6):788-795. https://doi.org/10.1016/j.annemergmed.2021.05.023
- Burnett AM, Watters BJ, Barringer KW, Griffith KR, Frascone RJ. Laryngospasm and hypoxia after intramuscular administration of ketamine to a patient in excited delirium. Prehospital Emergency Care. 2012;16(3):412-414. https://doi.org/10.3109/10903127.2011.640766
- Sullivan N, Chen C, Siegel R, Ma Y, Pourmand A, Montano N, Meltzer A. Ketamine for emergency sedation of agitated patients: A systematic review and meta-analysis. The American Journal of Emergency Medicine. 2020;38(3):655-661. https://doi.org/10.1016/j.ajem.2019.11.007
- Friedman MS, Saloum D, Haaland A, Drapkin J, Likourezos A, Strayer RJ. Description of adverse events in a cohort of dance festival attendees with stimulant-induced severe agitation treated with dissociative-dose ketamine. Prehospital Emergency Care. 2021;25(6):761-767. https://doi.org/10.1080/10903127.2020.1837311
- Cole JB et al. A prospective study of ketamine versus haloperidol for severe prehospital agitation. Clinical Toxicology. 2016;54(7):556-562. https://doi.org/10.1080/15563650.2016.1177652
- Lin J, Figuerado Y, Montgomery A, Lee J, Cannis M, Norton VC, Calvo R, Sikand H. Efficacy of ketamine for initial control of acute agitation in the emergency department: A randomized study. The American Journal of Emergency Medicine. 2021;44:306-311. https://doi.org/10.1016/j.ajem.2020.04.013
- Lipscombe C, Akhlaghi H, Groombridge C, Bernard S, Smith K, Olaussen A. Intubation rates following prehospital administration of ketamine for acute agitation: A systematic review and meta-analysis. Prehospital Emergency Care. 2022;1-15. https://doi.org/10.1080/10903127.2022.2108178
- Manasco AT, Stephens RJ, Yaeger LH, Roberts BW, Fuller BM. Ketamine sedation in mechanically-ventilated patients: A systematic review and meta-analysis. Journal of Critical Care. 2020;56:80-88. https://doi.org/10.1016/j.jcrc.2019.12.004
- Jung H, Lee J, Ahn HY, Yang JH, Suh GY, Ko RE, Chung CR. Safety and feasibility of continuous ketamine infusion for analgosedation in medical and cardiac ICU patients who received mechanical ventilation support: A retrospective cohort study. PloS One. 2022;17(9). https://doi.org/10.1371/journal.pone.0274865
- Chan K, Burry LD, Tse C, Wunsch H, De Castro C, Williamson DR. Impact of ketamine on analgosedative consumption in critically ill patients: A systematic review and meta-analysis. The Annals of Pharmacotherapy. 2022;56(10):1139-1158. https://doi.org/10.1177/10600280211069617
- Clayton GC. Society of Academic Emergency Medicine. Seizure & Status Epilepticus. Available at: https://www.saem.org/about-saem/academies-interest-groups-affiliates2/cdem/for-students/online-education/m4-curriculum/group-m4-neurology/seizure-status-epilepticus. Accessed December 27, 2022.
- Farkas J. The Internet Book of Critical Care. Status Epilepticus. Available at: https://emcrit.org/ibcc/sz/. Accessed December 27, 2022.
- Ochoa JG, Kilgo WA. The role of benzodiazepines in the treatment of epilepsy. Current Treatment Options in Neurology. 2016;18(4):18. https://doi.org/10.1007/s11940-016-0401-x
- Alkhachroum A et al. Ketamine to treat super-refractory status epilepticus. Neurology. 2020;95(16):2286-2294. https://doi.org/10.1212/wnl.0000000000010611
- Fang Y, Wang X. Ketamine for the treatment of refractory status epilepticus. Seizure. 2015;30:14-20. https://doi.org/10.1016/j.seizure.2015.05.010
- Göksu E, Kılıç D, İbze S. Non-invasive ventilation in the ED: Whom, When, How? Non-invasive ventilation in the ED: Whom, when, how? Turkish Journal of Emergency Medicine. 2018;18(2):52-56. https://doi.org/10.1016/j.tjem.2018.01.002
- Farkas J. The Internet Book of Critical Care. Noninvasive Respiratory Support. Available at: https://emcrit.org/ibcc/support/. Accessed December 28, 2022.
- Verma A, Snehy A, Vishen A, Sheikh WR, Haldar M, Jaiswal S. Ketamine use allows noninvasive ventilation in distressed patients with acute decompensated heart failure. Indian Journal of Critical Care Medicine. 2019;23(4):191-192. https://doi.org/10.5005/jp-journals-10071-23153
- Goyal S, Agrawal A. Ketamine in status asthmaticus: A review. Indian Journal of Critical Care Medicine. 2013;17(3):154-161. https://doi.org/10.4103/0972-5229.117048
- Agrawal A, Shrivastava J. Intravenous ketamine for refractory bronchospasm precipitated by H1N1 infection. Frontiers in Pediatrics. 2014;2:24. https://doi.org/10.3389/fped.2014.00024
- Calleja-Alarcón S, Sánchez-Hurtado LA, Romero-Gutiérrez L, Guerrero-Escobar JC, Ávila-García JE. Ketamine as a treatment of bronchospasm due to an anaphylaxis. A case report. Revista Médica del Instituto Mexicano del Seguro Social. 2022;60(3):356-360. PMID: 35763441
- Goyal S, Anand, S. Ketamine as a bronchodilator and antiepileptic in organophosphorus poisoning. Pediatric Oncall Journal. Available at: https://www.pediatriconcall.com/pediatric-journal/view/fulltext-articles/955/J/0/0/502/0. Accessed December 28, 2022.
- Jarvis JL, Lyng JW, Miller BL, Perlmutter MC, Abraham H, Sahni R. Prehospital drug assisted airway management: An NAEMSP position statement and resource document. Prehospital Emergency Care. 2022;26(1):42-53. https://doi.org/10.1080/10903127.2021.1990447
- Weingart SD, Trueger NS, Wong N, Scofi J, Singh N, Rudolph SS. Delayed sequence intubation: A prospective observational study. Annals of Emergency Medicine. 2015;65(4):349-355. https://doi.org/10.1016/j.annemergmed.2014.09.025
- Feder A et al. A randomized control trial of repeated ketamine administration for chronic posttraumatic stress disorder. The American Journal of Psychiatry. 2021;178(2):193-202. https://doi.org/10.1176/appi.ajp.2020.20050596
- Whittaker E, Dadabayev AR, Joshi SA, Glue P. Systematic review and meta-analysis of randomized controlled trials of ketamine in the treatment of refractory anxiety spectrum disorders. Therapeutic Advances in Psychopharmacology. 2021;11. https://doi.org/10.1177/20451253211056743
- McGirr A, Berlim MT, Bond DJ, Fleck MP, Yatham LN, Lam RW. A systematic review and meta-analysis of randomized, double-blind, placebo-controlled trials of ketamine in the rapid treatment of major depressive episodes. Psychological Medicine. 2015;45(4):693-704. https://doi.org/10.1017/s0033291714001603

Jonathan Mohnkern, BS, FP-C, CP-C, NRP, has worked in the EMS field for the past eight years with a background in rural, suburban, and urban settings. He currently operates as a 911 and transport paramedic in Upstate NY. Jon holds a bachelor’s degree in biology and psychology, has experience in EMS management and tactical medicine, and is a current medical non-commissioned officer in the New York Army National Guard. Jon is currently in medical school as a first-year medical student and is passionate about critical care, pre-hospital medicine, and EMS education.
