The 3P’s of Airway Management
Introduction
It is not enough to merely be able to intubate; that is, perform the physical skill of instrumenting the airway and placing an endotracheal tube. Too often, prehospital and emergency clinicians find themselves in situations where mere intubation is not necessarily the most effective and important intervention being performed, and by ignoring the possibility of being presented with any number of contingencies, they fail to manage the patient effectively.
Contingency planning is not just an important aspect of airway management, it is an essential component of patient care. The inherent nature of prehospital and emergency medicine almost guarantees that something will go wrong or not according to plan. Even the most well-researched protocols and innovative devices can be disrupted or confounded in those environments. The patient will not always present in a “textbook” manner, and therefore these clinicians will have to be able to access tools, techniques, and procedures that enable them to take appropriate action when things are not quite straightforward. What this does for prehospital and emergency clinicians is it enables them to work through solutions as they are presented with difficult and, in some cases, lethal situations as they manage the airway.
The decision to intubate is relatively straightforward, and the criteria are quite clear:
- Is the patient able to maintain their own airway?
- Is the patient able to ventilate effectively?
- Is the patient able to oxygenate effectively?
- Is the patient expected to acutely deteriorate to the point that failing to manage the airway will create future complications?
If any single or combination of the aforementioned criteria is met, a prudent clinician may make the decision to intubate the patient. But this does not exactly solve any problems and could potentially complicate an already complex clinical picture.
The point is the aforementioned criteria are usually present within the broader context of one or more of the following situations, also known as the 3P’s of Airway Management:
- Physically Difficult Airway
- Physiologically Difficult Airway
- Psychologically Difficult Airway
Deliberate contingency planning before encountering these difficult situations is essential to the reduction of morbidity and mortality. The framework for that contingency planning does not have to be overly complicated, in fact that could potentially exacerbate the situation. Simple but effective should be the goal.
A suggested framework to use to outline difficult airway contingency planning would include:
- Know Your Situation
- Know the Key Threats
- Identify and Prioritize Resources/Responses
- Draft/Communicate a Plan
- Refine and Execute the Plan
Contingency planning is something that is done far in advance of the patient presenting in extremis. This is where clinicians have the opportunity to get the predictable things right so that they can better respond to the unpredictable elements that are likely to be present. The predictable elements are things like preparing equipment (making sure batteries are fresh and charged) and ensuring all secondary and tertiary procedures are prepared and can be put in place without delay. Getting the predictable right also includes briefings prior to the start of shift or following the alert that a patient is on their way in. This will prove to be invaluable in the event that a patient presents in the midst of a psychologically difficult airway. The things that are unpredictable are the things that can disrupt our best laid plans. The patient’s acuity may be worse than we anticipated; the “best airway guy” may not be available; and we may be operating within a context that can create more problems for us later. By taking the time to prepare and lay out your contingencies, you are better equipped to respond when “things go wrong.” This is not limited to equipment and procedures, but the clinician’s cognitive performance. Contingency planning also allows for clinicians to keep a positive mindset when things start going wrong… because they planned for things to go wrong, and therefore are not surprised and caught off guard when that becomes reality. The positive mindset comes from not being caught unaware and without an answer to the problem. The clinician, and the team, will already know what is coming up next. The cognitive load is drastically reduced and allows for the headspace to think big-picture instead of being caught in the minutia and weeds of a high stress situation. This can provide for resilience and protect morale in situations that would mentally break those who find they are ill prepared to respond effectively amidst the chaos of a difficult airway. Well thought out contingencies ensure the execution of the plan is less stressful.
Know the Key Threats
In airway management, three potential threats can lurk beneath the surface of what would otherwise be a straightforward airway management scenario. Hypotension, hypoxia, and multiple attempts are well known to contribute to mortality and morbidity in airway management. The failure to identify and address these threats before attempting intubation can lead to several untoward adverse events, some of which include anoxic brain injury or cardiac arrest.
Hypoxemia
Hypoxemia alone can indicate advanced airway management, but it can also threaten the possibility of a good outcome. It can present secondary to hypoventilation, which would imply that not enough oxygen is getting into the lungs and, therefore, the bloodstream; or it can present secondary to impairment of gas exchange/alveolar-capillary function (e.g., cardiogenic shock, PE, ARDS, pneumonia).
Hypoventilation is relatively easy to correct, a clinician would just increase minute volume by ensuring adequate rate and tidal volume. Add to that supplemental oxygen to increase the FiO2, and the patient should respond favorably. If the patient does not respond, then it should be assumed that some form of shunt physiology is present inhibiting normal alveolar-capillary gas exchange. Preoxygenation may be difficult, and peri-intubation desaturation/hypoxia is a real risk. These patients have little oxygen left in their physiologic reserves and are in a precarious situation.
Correction of hypoxemia in the presence of shunt physiology includes two objectives: fully saturating the red blood cells and increasing arterial oxygen content (PaO2). Depending on the severity of the shunt, this could prove to be relatively straightforward or quite complex if it can be accomplished in more severe cases.[i]
Preoxygenation strategies currently include the use of passive/apneic oxygenation via a nasal cannula at max flow (15lpm) coupled with a secondary device such as a non-rebreather mask or bag valve mask (for those with poor respiratory effort). The use of passive/apneic oxygenation for preoxygenation during airway management is a widely known and accepted method for sustaining oxygen saturation levels during airway management procedures, regardless of the patient’s ventilatory status.[ii] CPAP/BiPAP can also be an effective preoxygenation method, but it is contingent on patient cooperation and adequate mental status.2
Regardless of the selected preoxygenation strategy, the goal is to prolong the safe apnea time by increasing oxygen saturation of RBCs and oxygen capacity in the lungs by de-nitrogenating the alveoli. Safe apnea time is the time it takes for a patient to desaturate during an airway management procedure. This time is highly variable, and there are several factors that can influence this, but the general idea is that the higher the PaO2 and SpO2 are, the longer it will take for the patient to desaturate to a level dangerous enough (88%-90%) as to prompt abandoning the intubation attempt and re-oxygenating the patient until oxygen levels are sufficient to support another attempt.2
Evidence provided by Weingart et al., suggests that while the time to desaturation can be extended with the implementation of a sound preoxygenation strategy that includes the previously mentioned elements, the point at which the patient begins to desaturate rapidly is more important. The risk of desaturation is more closely related to their oxygen saturation prior to the intubation attempt. A patient is at relatively low risk for desaturation with a SpO2 between 94-98% and could potentially maintain that level of saturation for 6-8 minutes.2 However, a patient who is saturating at 88% (by definition already hypoxemic) will not only desaturate to much more dangerous levels, they may do so much faster. When performed intentionally and goal-directed, preoxygenation provides the patient with a margin of safety during airway management procedures that protect against morbidity and mortality.2
Hypotension
Pre-intubation hypotension is defined as SBP < 90 prior to the intubation attempt. Available evidence suggests that it complicates 25% of patients requiring airway management and carries a significant risk of post-intubation cardiac arrest.[i] It is an independent predictor of in-hospital mortality. In one study, 30% of cases where a patient underwent airway management in the presence of pre-intubation hypotension resulted in cardiovascular collapse.
The causes of pre/post-intubation hypotension are not perfectly understood, but there are three apparent possibilities as to why it occurs. One possibility is the negative inotropic effect coupled with peripheral vasodilation following the administration of induction agents. Another possibility is that positive pressure ventilation is causing increased intrathoracic pressure that results in reduced venous return to the heart and, therefore, a reduction in cardiac output.3 The last possible explanation for post-intubation hypotension may be the most “makes sense” explanation.
Current evidence suggests a reduced or halted catecholamine response is secondary to the administration of induction agents. A patient in extremis is experiencing a sympathetic stimulation brought on by the understanding that they are in a dangerous situation and may be dying. This, in turn, leads to the release of endogenous catecholamines to increase heart rate and blood pressure (among other things). One basic premise of pharmacologically assisted airway management is to completely dissociate the patient in order to attenuate or reduce the discomfort and likely traumatic experience of being chemically paralyzed for intubation. If the patient is psychologically dissociated from their current circumstances (they no longer have awareness of their dire situation), the sympathetic stimulus is no longer there, and therefore, the release of endogenous catecholamines is halted, and hypotension soon follows.[ii]
Identifying hypotension is relatively straightforward. An SBP <90 would suggest that the patient is profoundly and dangerously hypotensive. If one were curious as to the severity of the shock state the patient is in, a shock index could be calculated. Divide the HR by the SBP, which will provide the clinician with a shock index. 0.8->1.0 is the range considered to be severe shock requiring immediate resuscitation. In airway management, a shock index between 0.8 and 1.0 indicates that the patient needs hemodynamic optimization and aggressive resuscitation before attempting intubation.4 Evidence suggests that aggressive fluid resuscitation and use of vasopressors (infusion or bolus dose) can ameliorate or temporize peri-intubation hypotension and make for safer physiologic conditions for intubation.14
Another measure to address pre/post-intubation hypotension, while not as popular and somewhat controversial, is to adjust the dosages of induction agents and paralytics. Specifically reducing the dosage of the induction agent and increasing the dose of the paralytic.3 Understanding this concept warrants a discussion of pharmacokinetics and pharmacodynamics and the patient’s influence of those two elements in the setting of shock. As previously mentioned, a patient in shock is receiving the benefit of sympathetic stimulation and endogenous catecholamine release to support oxygen delivery and blood flow to the critical core and organs. The body is ensuring the perfusion of the heart, lungs, and brain by shunting blood back to those areas, regardless of the etiology (vasoplegic, hemorrhagic, etc.).
In his presentation The Case of the Dying Soldiers, Dr. Michael Lauria presents a logical framework for conceptualizing this. Shock states are usually “low flow” states, meaning that there is reduced cardiac output (in most cases), lower circulating volume (secondary to fluid loss, bleeding, and shunting), and lower drug redistribution (due to shunting from fats and muscle tissues). Also, patients in shock are often acidotic, which negatively influences the performance of the medications. All of this serves to essentially “super-charge” the actions of all induction agents for several reasons: there is a greater concentration of the medication than there is in a euvolemic or hemodynamically stable patient; the solution is moving slower and is distributed over a longer period of time, and the bloodstream stays concentrated with the medication for a much longer period of time. The supercharged medication will revisit the brain and CNS more often and for a longer period of time as it is slowly redistributed and metabolized, exacerbating the untoward effects of our induction agents. When dosed at normal RSI dosages, all induction agents will reduce the blood pressure and, in some cases, potentiate a quick and profound onset of hypotension.[iii]
Paralytics are just the opposite. Rather than their action being super-charged due to the pharmacodynamics/kinetics of shock states, their action is much slower to onset. Paralytics are cardiac output dependent on distribution to the muscles and receptors needed to achieve effective paralysis.5 As noted above, in shock, medications are much slower to reach the muscles, and when dosed at “normal” RSI doses, much less medication is reaching the receptors, and paralysis will be delayed, potentially complicating an emergent situation. To combat this, doubling the dose may be a solution to ensuring an adequate amount of medication is distributed in a timely manner to achieve optimal intubating conditions.
Multiple Attempts
The risk of multiple attempts in airway management cannot be overstated. Multiple attempts of instrumenting and placing an ET tube are directly correlated to adverse events such as hypoxemia, tube misplacement (esophageal intubation), and cardiac arrest.[i] The data also suggest that the more attempts made at intubation, the more likely these events are to occur.6 More than three attempts predict with near 100% certainty that an adverse event will occur.
There is not a silver bullet solution for fixing the problem of multiple intubation attempts. Training and simulation can only take a clinician so far. However, several adjuncts exist that can aid in first-pass success by working around some of the physical barriers to effective instrumentation of the airway and visualization of the glottic opening.
Ramping and positioning the patient’s ear to the sternal notch is of great benefit in obtaining a view of the glottic opening.2 This adjunct is designed to change the angle or visual axis a clinician has to contend with during intubation. With a patient laying supine, the visual axis is nearly 90 degrees, meaning the clinician performing the procedure is looking straight down into the oropharynx and then lifting the tongue and jaw enough to uncover the glottic opening, which is (at this angle) perpendicular to the mouth. Ramping (using pillows and blankets to elevate shoulders and head) and bringing the ear to the sternal notch places the mouth more in line with the glottic opening and greatly reduces the effort needed to obtain a glottic view, especially when the airways are more anterior.
Suction-assisted laryngoscopy airway decontamination (SALAD) is another rather effective method in clearing the view of the glottic opening in the presence of a soiled airway. Emesis, blood, water, and other fluids can be present in the oropharynx and hypopharynx, which can completely or partially obstruct the view of the glottic opening. The use of a DuCanto suction catheter and the SALAD technique reduces the time to clear the oro/hypopharynx of fluids. This technique involves leading the laryngoscope with a large-bore suction catheter and decontaminating the airway as you progress through the landmarks, then leaving the suction catheter in place during the intubation attempt, which serves to keep the visual field clear while attempting to place an ET tube should the patient be actively bleeding into the hypo/oropharynx or if the patient vomits during the procedure.
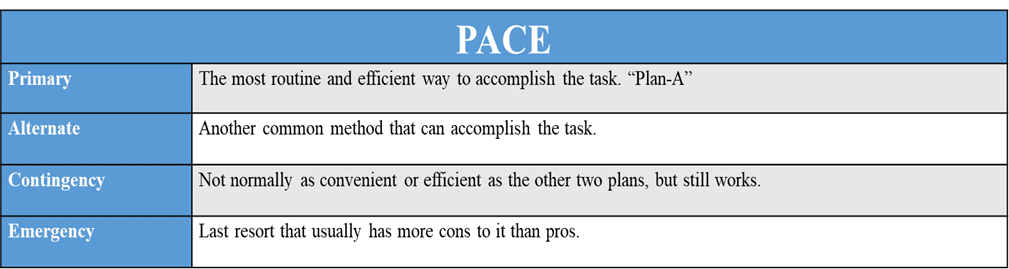
PACE is not something that can be done in the heat of the moment; attempting to do so would be to invite disaster. PACE is part of the pre-planning process that is most effective when completed early, and the various responses are rehearsed and discussed regularly. They should be simple enough to fit on quick reference cards that can be carried in a pocket for easy retrieval.
What does PACE planning do for a clinician? It allows the team to plan for things to go wrong and keep a positive mindset when they do. Resilience is the key in these situations as there is a psychological factor to effective resuscitation performance. Moreover, when things do not go according to plan, the team already knows how to respond and what is coming next because this was taken care of in the pre-planning phase.
Communicate and Draft the Plan
Well-thought-out plans ensure that the execution of the plan is less stressful. Proper and effective communication of the plan prior to the patient’s presentation (either arrival in the ED or flight crew arrival at the bedside) is also essential to ensure the successful execution of advanced airway management.
Checklists are an effective method for communication of the plan and drafting the plan. They should be an adjunct to a sound clinical plan of patient management. Every effort should be made to ensure they are prescriptive/restrictive in nature to remove the team’s ability to pivot away or toward resuscitation elements that may affect a good outcome. Communication and checklists should be as simple as they can possibly be. Introducing complicated plans/solutions into complex situations ensures that the situation’s chaos will be amplified, not controlled. Team members should know their roles, communicate their understanding, and ask any/all clarifying questions necessary to ensure the safe and effective execution of their tasks during the resuscitation.
Know Your Situation: The 3P’s of Airway Management
Knowing your situation is key to selecting the correct clinical management plan to deal with a difficult airway effectively. Each difficult airway scenario presents a unique set of challenges on its own and, when presented together, can present even the most experienced clinicians with an incredibly difficult airway management scenario. We have decent tools to identify the need for intubation and the degree of difficulty we may encounter. Our problem is that we sometimes fail to place that difficulty in its proper context. It may only be limited to identifying and implementing strategies to reduce the difficulty associated with physically (anatomically) difficult airways, which leaves little room for consideration of other issues that may make airway management more difficult. Failing to assess and appreciate your situation completely could lead to a fatal error of not looking for/identifying a key risk factor and inadvertently contributing to morbidity and/or mortality.
Physically Difficult Airways
As the name would imply, these are patients presenting with a need for airway management along with some physical difficulty in instrumenting the airway, obtaining a view of the glottic opening, or placing an endotracheal tube. Physically difficult airways present in any one of the following ways:
- Disrupted anatomy (usually from trauma)
- Congenital issues
- Soiled from vomit/blood/fluids
- Pediatrics
- Bariatrics
- Burns
The key threats to mitigating physically difficult airways are multiple attempts and hypoxia. Positioning and a good preoxygenation strategy may assist with mitigating those threats. A PACE plan for physically difficult airways may include the following:
- Physically Difficult – Position and Preoxygenate
- P: Position/Ramping w/ standard preoxygenation strategy
- A: Upright CPAP/BiPAP for preoxygenation (if cannot lay flat at all)
- C: SALAD technique if soiled airway.
- E: SGA or Cric
Physiologically Difficult Airways
Research on managing the airway in critically ill patients suggests that outcomes are poorer when intubation is attempted prior to optimizing the patient’s hemodynamics. Pre-oxygenation simply is not enough to stabilize a patient to the point that a poor outcome can be avoided.
Hemodynamic instability can present secondary to a primary medical cause or a primary traumatic cause (e.g., hemorrhage). Oxygen delivery is our primary concern despite the cause, and we can address the physiologic issues by enhancing and optimizing each part of oxygen delivery.
Resuscitation does not begin or end with intubation. Keeping this in mind, an approach to optimizing oxygen delivery would involve:
- Maximizing arterial oxygen content through increasing FiO2, oxygen storage capacity (functional reserve capacity), and the diffusion of oxygen from the alveoli to the bloodstream.
- Maximizing oxygen-carrying capacity by providing blood transfusions to ensure hemoglobin and RBC levels are appropriate and can move the oxygen to the tissues.
- Optimizing cardiac output by appropriately targeting and optimizing preload, afterload, and contractility with the use of vasopressors and fluid challenges (as appropriate).
Once the need for intubation is identified in the presence of physiologic derangement, a plan should be implemented to ensure the safest possible conditions for intubation by hemodynamically optimizing the patient to tolerate the procedure without hypotension, bradycardia, or cardiac arrest. A PACE plan for this difficulty would include:
- Physiologically Difficult Airway – Resuscitate Before You Intubate
- P: Fluid bolus and push-dose pressors prn to stabilize hemodynamics
- A: Pack, Wrap, Bind, and Hang (hemostatic resuscitation) OR initiate pressor infusion.
- C: Adjust drug dosing for profound shock
- E: Crash (peri-arrest intubation)
Psychologically Difficult Airways
Invariably, at some point in a clinician’s career, he or she will be confronted with a situation in which all pre-planning and preparation completely fall apart. The term for this would be going “beyond all contingencies.” It is rare if contingency planning was executed and refined prior to the incident that a single element would be the causative factor in things going awry. Things usually go “beyond all contingencies” for one of the following reasons:
- Contingency planning was not deep enough to account for multiple variables.
- The clinician is unable to recover from a mistake and is caught in a negative feedback loop.
- The clinician cannot break a cycle of paralysis by analysis and cannot make decisions to keep the resuscitation moving forward.
The reasons a resuscitation may begin to derail are many, but most of them can be attributed to the friction and the inherent nature of prehospital and emergency medicine. There are three points of friction that can turn even a simple airway management situation into a cognitive crisis if the tools are not in place to manage the difficulties and take care of the patient effectively.
People are perhaps the greatest friction point in resuscitation. In these situations, there are people interacting with other people in a high-stakes/high-consequence environment. Each of the clinicians brings an element of friction to the bedside with them that can be exposed under varying levels of stress:
- Stressed out and/or burned out
- Tired/Fatigued
- Mal-nourished
- Skill and/or knowledge deficiencies
- Poorly practiced / no recency of experience
- Forceful w/ different opinions (simply not a team player)
Another area of friction is the environmental context within which clinicians are operating. A flight team may encounter enormous friction at a sending facility by initiating advanced airway management when the facility staff does not see a reason to do so. That flight team is now operating in a non-permissive environment where personnel support could be lacking, and there may be a threat of disciplinary actions against the team for executing the procedure. Prehospital teams may be operating on the side of a road with minimal support or in extremes of environmental factors (temperature and weather). Any number of factors can contribute to the environment taking it from a “permissive/supportive” environment to a “non-permissive/hostile” environment. Technology is the final friction point in resuscitation. As technology becomes more complicated, humans may find difficulty in adapting to and interacting with that technology. The opposite is also true where equipment may be outdated and unreliable so as to impact a resuscitation scenario negatively. Wegersma, in 2011 opined that 38% of all critical care transport is complicated by some failure of technology. That is batteries failing, power sources failing, the absence of the correct equipment, and/or the inability of the transport team to employ the technology effectively.
These types of issues do not suddenly erupt into chaos…as a general rule. Instead, the onset is often slow and insidious, and only an astute and emotionally detached team leader (e.g., one who is not actively involved in contributing to that chaos) will be able to identify the following characteristics of a situation moving beyond all contingencies:
- The team cannot/will not work together.
- No one has stepped up and assumed leadership of the situation.
- Poor/Non-existent communication.
- Poor decision making (e.g., over committing to intubation and executing several attempts).
How can some teams operate well when things have gone beyond all contingencies and others cannot? Basic principles of teamwork and crew resource management may provide some explanation.
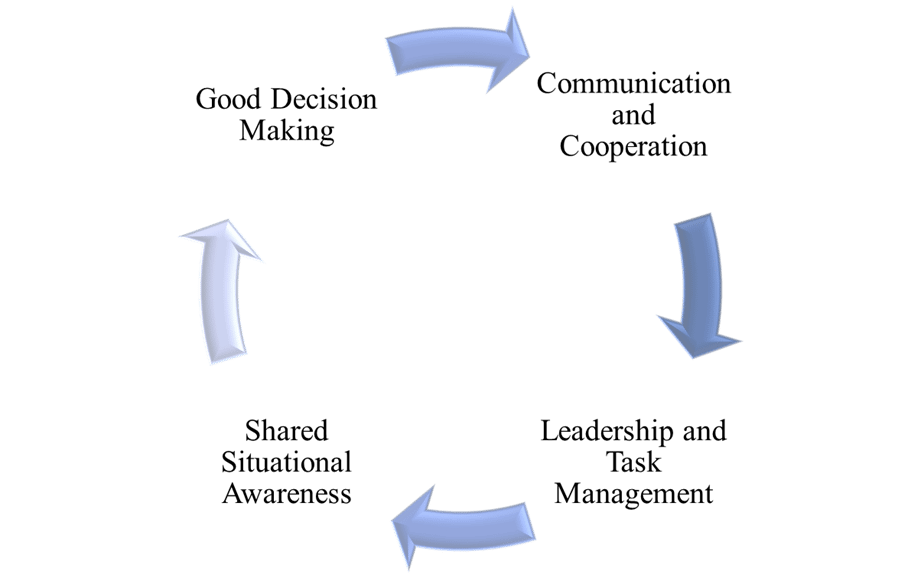
- Communication and Cooperation: The team lead communicates the vision and goals. “We will be intubating this patient, and we will need to work to ensure that we do it without hypotension and hypoxia on the first attempt.” The individual team members will then communicate their 1.) understanding of their role. 2.) Questions and concerns. Ensuring the time for questions and concerns is crucial to removing potential friction points that may arise in the stress of the situation.
- Leadership and Task Management: The team lead has to stay out of the weeds and maintain a big picture view of what is taking place. If an individual is intubating, they cannot possibly maintain the needed situational awareness to keep things moving forward. The lead needs to be looking around making sure the patient is handling the procedure and then thinking about the next phase of the procedure. Control the environmental context by giving people jobs to do and removing those who do not need to be in the room or area.
- Situational Awareness: The team knows the vision, and the leader must be aware of and communicate where the roadblocks are and provide the information that the team needs in order to keep things moving forward. Sometimes in airway management situations not everyone understands what is going on, why things are being done in a certain way, and have no contextual reference for the procedures that are being performed. Good team leadership ensures that everyone is operating from the same sheet of music and shared consciousness.
- Good Decision Making: The ability to make decisions needs to be pushed as far down and forward as possible and team members have to be free to do what they know needs to happen. Of course, this is predicated on the fact that there is good two-way, closed-loop communication taking place. There are several instances where people ask for permission or confirmation/validation that their decision is correct. This serves to add unnecessary noise to the overall situation, and to get ahead of this, leaders should allow people to make the decision to do what they know needs to happen. The leader should set the priorities for what needs to take place, but needs to assume an “eyes on, hands off” posture to let people make the right decision on how to execute on it.
What would a contingency plan for psychologically difficult situations look like?
- Psychologically Difficult Airways: Beyond All Contingencies
- P: Establish leadership and communicate a plan. Get a checklist out.
- A: Allow someone else to lead, and you perform skills.
- C: Remove ALL non-essential personnel and reestablish/reassign leadership and tasks. Reassign people to tasks they are better suited for.
- E: Medical Director contact. Move to the ambulance/aircraft and execute.
Conclusion
Successful airway management requires deliberate and well-thought-out preplanning in order to ensure the best possible chance of intubation success and a good patient outcome. PACE planning can serve as a framework for evaluating and responding to the likely contingencies and problems a clinician could encounter during advanced airway management. Addressing hypotension, hypoxia, and the possibility of multiple attempts before initiating airway management serves to create the safest possible conditions for intubation and can work to ensure the patient can tolerate the procedure despite physical difficulty or physiological derangement.
References
[1]Jarrod, M. (2015). The Physiologically Difficult Airway. West J Emerg. Med., 1109-1117.
[1] Weingart, S. (2012). Preoxygenation and Prevention of Desaturation During Emergency Airway Management. Annals of Emergency Medicine, 165-175.
[1]Heffner. (2012). Predictors of the complication of post-intubation hypotension during emergency airway management. Journal of Critical Care, 587-593.
[1] Heffner, A. (2012). The frequency and significance of postintubation hypotension during emergency airway management. Journal of Critical Care, 417-419.
[1] Lauria, M. (2015). “The Case of the Dying Soldiers.” Youtube. April 15, 2018. https://youtube.com/watch?v=TeNOIN1oBcE [1]Sackles, J. (2013). The Importance of First Pass Success When Performing Orotracheal Intubation in the Emergency Department. Acad Emerg. Med, 71-78.

Cody Winniford, BA, EMT-P, CCP-C, FP-C
Cody has been in EMS for 18 years, serving in both military and civilian settings. His professional experiences include serving as an educator for initial paramedic instruction programs, clinical manager, EMS operations manager, and EMS Operations Director. He is currently serving as a flight paramedic with PHI Air Medical and volunteers for the education committee for the ICAPP.
